PharmaCare Newsletter
February 2026 PharmaCare Newsletter
On this page:
Print off the PDF of this PharmaCare Newsletter, and post it in your pharmacy for staff to read!
February PharmaCare Newsletter (PDF)
Find past issues on the newsletter search page.

Q: What is the role of venlafaxine (Effexor XR, generics) in the management of menopause-associated hot flashes?
A: The answer is in the current edition of PAD Refills. Make sure to subscribe so you don’t miss out on news and updates!
National Pharmacare Plan launches March 1
The provincial universal National Pharmacare Plan (Plan NP) was created under the Drug Plans Regulation on January 29, 2026. In addition, the pricing of insulin as a PharmaCare benefit will be regulated under the Drug Price Regulation and subject to the Maximum Pricing Policy, and the Full Payment Policy through an amendment to the Provider Regulation.
Starting March 1, Plan NP will provide 100% coverage of select diabetes medications, menopausal hormone therapy (MHT), and contraceptives. The federal government contributes funding for national pharmacare.
The pricing of insulin as a PharmaCare benefit will be regulated under the Drug Price Regulation and subject to the Maximum Pricing Policy, and the Full Payment Policy through an amendment to the Provider Regulation. Insulin was previously unregulated and covered at retail price. This change will go into effect March 1, 2026.
All B.C. residents enrolled in MSP will be eligible for Plan NP coverage. Plan NP coverage is provided at the pharmacy and processed in PharmaNet, as with all BC PharmaCare plans. Exceptional coverage will be available for clients in the MSP coverage wait period.
Expanded coverage for certain diabetes-related devices and supplies will begin on April 1, 2026. More details to come in the March 2026 PharmaCare Newsletter.
Plan NP benefit lists
Health providers can review the Plan NP benefit lists now on these new web pages:
The contraceptives now covered under Plan Z will be covered under Plan NP.
Some benefits are subject to Low Cost Alternative (LCA) pricing. The public is being encouraged to ask their pharmacist or prescriber to adapt to or prescribe fully covered benefits.
PharmaCare's Full Payment Policy applies to Plan NP benefits with 100% coverage, including insulins. This means pharmacies cannot charge a client for the medication or any service associated with the dispense. Insulin was previously unregulated and covered at retail price. This change will go into effect March 1, 2026.

Need information on MHT? Contact the BC Provincial Academic Detailing (PAD) service to schedule a session on Medications for menopause-associated vasomotor and genitourinary symptoms.
You can also read the PAD Refills Newsletter topic for January 2026, What is the role of Duavive in the management of menopause symptoms?
Special Authority coverage
Several Plan NP diabetes benefits will continue to require Special Authority (SA). Once SA is approved, the benefits have 100% coverage and the Full Payment Policy applies (LCA pricing may apply for some products).
No MHTs or contraceptives will require SA.
Pharmacists cannot apply for SA for Plan NP benefits; however, they can draft an SA request for a prescriber to review, sign and submit.
On March 6, 2025, the Province of B.C. was the second province (after Manitoba) to sign an agreement with the Government of Canada for the implementation of national pharmacare. Agreements were signed shortly after with Prince Edward Island and Yukon.
Resources
- Drug Plans Regulation
- Provider Regulation
- PharmaCare Policy Manual, Section 5.10: Full Payment Policy
- PharmaCare Policy Manual, Section 5.6: Maximum Pricing Policy
- Low Cost Alternative (LCA) program
- Special Authority (SA)
- BC Provincial Academic Detailing (PAD) service Medications for menopause-associated vasomotor and genitourinary symptoms
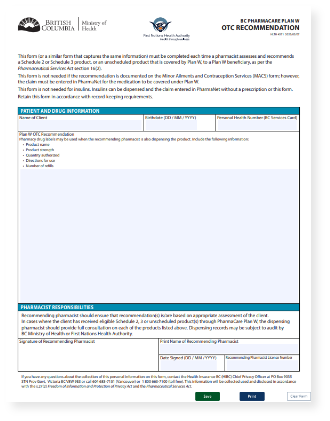
Updates to Plan W policy and OTC recommendation form
In response to feedback from clients and health care providers, PharmaCare has updated the PharmaCare Policy Manual, Section 7.12: First Nations Health Benefits (Plan W) and the Plan W OTC Recommendation form (PDF, 548KB) to help dispensing and non-dispensing pharmacies more easily recommend OTC items to Plan W clients.
The updates mean that:
- A Plan W OTC benefit can be recommended by a pharmacist and dispensed at a different pharmacy, under the recommending pharmacist’s licence, similar to Minor Ailments and Contraception Service (MACS) prescriptions
- A Plan W OTC recommendation can be documented on any form, as long as it includes the information required on the OTC recommendation form
- The client’s signature is no longer required, and pharmacists can authorize refills
Free, 1-hour online course
The Ministry of Health, First Nations Health Authority (FNHA), University of British Columbia (UBC) and community pharmacy colleagues have collaborated to develop a provider-facing educational course regarding these changes. The course, Plan W OTC Recommendations: 2025 Updates, is now live and can be accessed at no cost.
The course highlights how these changes are meant to support culturally safe provision of services for FNHA clients and provides examples of how pharmacists can implement these changes in their daily practice. The course counts as one hour towards the minimum three hours of learning related to Indigenous Cultural Safety, Cultural Humility, and Anti Racism required annually by the BC College of Pharmacists.
Resources
- Plan W OTC Recommendations: 2025 Updates – one-hour online course
- PharmaCare Policy Manual, Section 7.12: First Nations Health Benefits (Plan W)
- Minor Ailments and Contraceptives Service (MACS)
- Plan W OTC Recommendation form (PDF, 548KB)
PharmaCare Trends 2024/25
The latest edition of PharmaCare Trends 2024/25 (PDF, 781KB) is now available. The report highlights progress in delivering an effective, balanced and responsive PharmaCare program, with sections detailing expenditures by PharmaCare plan, the top ten drugs covered, formulary expansion, and more.
This document is published annually by the BC Ministry of Health. It provides information about the PharmaCare program for health researchers, government staff and the public.
Data in this publication is from the fiscal year 2024-2025 and reports on claims for drugs and medical devices and supplies for which PharmaCare contributed at least a portion of the cost.
Read previous editions of PharmaCare Trends on the PharmaCare publications web page.
Resources
New cultural safety learning opportunities at UBC CPPD
Registration is now open for three new Indigenous cultural safety learning opportunities at UBC Continuing Professional Development and Practice (CPPD). All courses and webinars are free and designed to support culturally safe pharmacy practice.
Indigenous Health Benefits (Online course – 1 credit)
This asynchronous online course provides an overview of Indigenous health benefits, including how pharmacists can support client access, navigate benefit structures, and promote culturally safe interactions with clients. Register at Uprooting Pharmacy – Indigenous Health Benefits. The course is available until January 14, 2027.
Barriers and Facilitators to Culturally Safe Practice (Webinar – 1 credit)
Join the online webinar designed to strengthen culturally safe pharmacy practice on February 12, 2026, from 12–1pm. This session explores how Western and Indigenous worldviews shape care in a pharmacy context. Register at Uprooting Pharmacy – Barriers and Facilitators to Culturally Safe Practice Webinar - Cultural Safety and Humility.
Bringing Together Traditional and Western Medicines (Webinar – 1 credit)
Expand your understanding of team‑based practice in this webinar on February 26, 2026, from 12–1pm. This session reviews the history of extractive science and biopiracy and how these legacies influence pharmacy practice today. Register at Uprooting Pharmacy – Bringing Together Traditional and Western Medicines Webinar - Cultural Safety and Humility.
Visit Indigenous Cultural Safety, Humility, and Anti‑Racism | Pharmsci to learn more.
Resources
- Indigenous Cultural Safety, Humility, and Anti‑Racism | Pharmsci
- Uprooting Pharmacy – Indigenous Health Benefits
- Uprooting Pharmacy – Barriers and Facilitators to Culturally Safe Practice Webinar - Cultural Safety and Humility
- Uprooting Pharmacy – Bringing Together Traditional and Western Medicines Webinar - Cultural Safety and Humility
Reminder: Pharmacist interviews about nicotine cessation support in B.C.
A Ministry-funded research study by the University of British Columbia continues to seek input from community pharmacists providing non-pharmacologic nicotine cessation support to patients in B.C.
Community pharmacists who complete a 30-minute one-on-one interview with the research team will receive a $50 honorarium for their participation. To take part in the study, contact Dr. Karen Dahri at karen.dahri@vch.ca. The goal of the interviews is to determine how community pharmacists in B.C. deliver non-pharmacologic nicotine cessation support to individuals who smoke and/or vape and related barriers and facilitators to providing this service.
B.C. community pharmacists can assess clients for nicotine dependence as part of the Minor Ailments and Contraception Services (MACS). They are encouraged to sign clients up for the BC Smoking Cessation Program, which covers the full cost of nicotine replacement therapy (NRT) products and some or all the cost of prescribed smoking cessation medications.
Pharmacists assessing clients for nicotine dependence are encouraged to enrol in the UBC Continuing Professional Development and Practice (CPPD) course MACS: Tobacco Use Disorder.
Resources
- Smoking cessation – BC PharmaCare
- Minor Ailments and Contraception Services (MACS) – BC PharmaCare
- Ministry of Health Research Seed Grant Program – UBC
- MACS: Tobacco Use Disorder – UBC CPPD
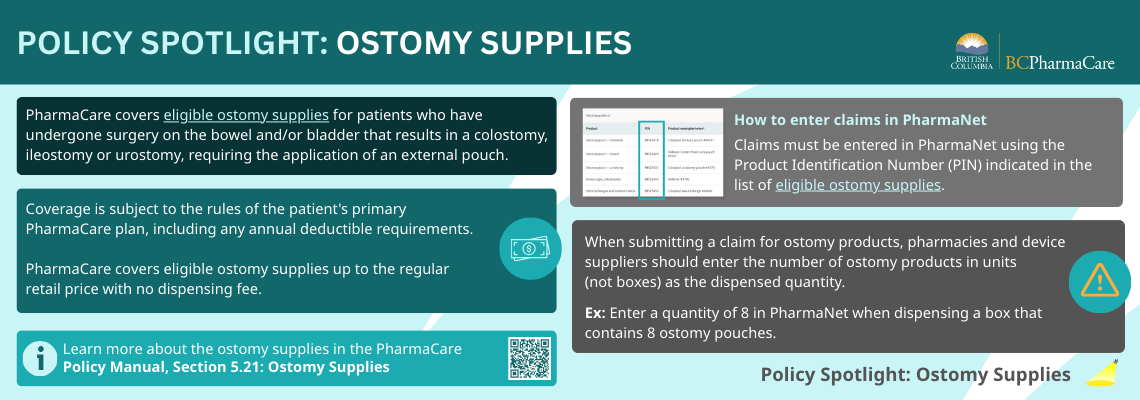
Reminder: Correct quantities of ostomy supplies
When submitting a claim for ostomy products, pharmacies and device suppliers should enter the number of ostomy products in units (not boxes) as the dispensed quantity.
For example, enter a quantity of 10 in PharmaNet when dispensing a box that contains 10 ostomy pouches. Using the correct unit of measurement will ensure accurate payment and patient records.
For more information, refer to Correct quantities for PharmaCare claims and the PharmaCare Policy Manual, Section 5.5: Correct Quantities Policy.
Resources

Policy Spotlight: Ostomy supplies
Resources
New poster: Your PharmaNet records. Your privacy.
The PharmaCare communications team has created a new poster for pharmacy clients about PharmaNet records.
The poster includes information about who can view a client’s PharmaNet records, what information is in their PharmaNet records, adding a password to their PharmaNet records, and accessing their records through Health Gateway.
Visit Your PharmaNet records (PDF, 115KB) to view and download the poster.
Resources
QuitNow program launches new referral portal
QuitNow has launched the new QuitNow Referral Portal to help healthcare providers, including pharmacists, refer clients for support with quitting or reducing smoking, vaping, and other forms of nicotine use. The new portal makes the referral process easier, faster and more secure, and strengthens continuity of care.
The QuitNow Referral Portal offers referring providers:
- A streamlined digital referral form—no faxing
- Enhanced security and privacy protections
- Tracking of referral status
- Client updates, such as if they’ve connected with QuitNow coaching services
- Access to research and training resources
It takes less than 10 minutes to create a provider account and start sending referrals. If you don’t find your pharmacy in the dropdown list, select “Other”. It takes less than two minutes to submit a referral for a client once your account is set up. Learn how by watching QuitNow’s two-minute instructional video.
QuitNow is a program for B.C. residents wanting to quit or reduce tobacco and nicotine use, delivered by the BC Lung Foundation on behalf of the B.C. government. The program offers free and confidential services to B.C. residents aged 10 and older.
The QuitNow Health Care Providers web page has resources, training opportunities and webinars to support providers with nicotine cessation counselling and treatment planning.
Pharmacists are always encouraged to sign people up for the BC Smoking Cessation Program, which covers the full cost of nicotine replacement therapy (NRT) products and some or all the cost of prescribed smoking cessation medications. Learn more at Smoking Cessation Program – information for health professionals.
Pharmacists assessing clients for nicotine dependence as part of a Minor Ailments and Contraception Service (MACS) are encouraged to enrol in the UBC Continuing Professional Development and Practice (CPPD) course MACS: Tobacco Use Disorder.
Resources
- QuitNow Referral Portal
- QuitNow Referral Portal: Create an account
- QuitNow instructional video: How to create a provider account
- QuitNow: Health Care Providers page
- Smoking Cessation Program – information for health professionals
RAT kits available free of charge until supplies run out
Pharmacies are encouraged to order RAT kits from distributors, available free of charge until supplies run out. Pharmacy distributors have stockpiled kits to be available to pharmacies and stores until the supply is exhausted or expired (i.e., late 2026).
Formulary and listing updates
Limited Coverage benefits: captopril (Noyada)
PharmaCare has added the following limited coverage item to the PharmaCare drug list. Special Authority approval is required for coverage.
| Drug name | captopril (Noyada) | ||
|---|---|---|---|
| Date | January 28, 2026 | ||
| Indication | The treatment of essential or renovascular hypertension, diabetic nephropathy, or congestive heart failure | ||
| DINs | 02543907 02543915 |
Strength & form | 5 mg/5 mL oral solution 25 mg/5 mL oral solution |
Regular benefit: ethambutol (Etibi)
PharmaCare has decided to cover the following drug as a regular benefit.
| Drug name | ethambutol (Etibi) | ||
|---|---|---|---|
| Date | February 4, 2026 | ||
| Indication | Treatment of all forms of tuberculosis, including tuberculous meningitis, caused by Mycobacterium tuberculosis | ||
| DIN | 00247960 | Strength & form | 100 mg tablet |
Your Voice: Input needed for drug decisions
The knowledge and experience of patients, caregivers and patient groups is integral to B.C.'s drug review process. If you know someone who is taking one of the drugs below or who has a condition any of the drugs treat, please encourage them to visit www.gov.bc.ca/BCyourvoice.
Your Voice is now accepting input on the following drugs:
| Drug | Indication | Input window | ||
| sarilumab (Kevzara®) | Polymyalgia rheumatica (PMR) in adults | January 28 to February 24 at 11:59 pm | ||
| pegcetacoplan (Empaveli™) | C3 glomerulopathy (C3G) or primary immune-complex membranoproliferative glomerulonephritis (IC-MPGN) in adults and adolescents aged 12 years and older | January 28 to February 24 at 11:59 pm | ||
| caplacizumab (Cablivi®) | Acquired thrombotic thrombocytopenic purpura (aTTP) in adults | January 28 to February 24 at 11:59 pm | ||
| vosoritide (TBC) | Achondroplasia in pediatric patients whose epiphyses are not closed | January 28 to February 24 at 11:59 pm | ||
About the PharmaCare Newsletter
The PharmaCare Newsletter is published on the first Wednesday of each month, with occasional mid-month releases. The PharmaCare Newsletter communicates drug listings, PharmaCare policy, PharmaNet procedures, and other pertinent information for PharmaCare providers and health care partners.
Information in previous newsletters is accurate as of the date it was published. Newsletters are not retroactively updated when policy, procedures or other information changes. Refer to the most recent mention of a topic for up-to-date information.
Search past newsletters on the Newsletter search page.
Subscribe
Enter your email address to subscribe to updates of this page.
 The PharmaCare Newsletter team works from the territory of the Lekwungen People, including the Songhees and Esquimalt Nations. Our gratitude extends to them, and all the Indigenous Peoples on whose territories and lands we build relationships.
The PharmaCare Newsletter team works from the territory of the Lekwungen People, including the Songhees and Esquimalt Nations. Our gratitude extends to them, and all the Indigenous Peoples on whose territories and lands we build relationships.
BC PharmaCare counts on pharmacy and device providers to practise cultural safety and humility.
To learn more, read Coming Together for Wellness, a series of articles by First Nations Health Authority (FNHA) and PharmaCare, and consider taking the online San’yas Indigenous Cultural Safety course.
Active advisories
spironolactone tablets; disopyramide capsules; olanzapine for injection; peginterferon alfa-2a (Pegasys®) injection
Visit Drug shortages for full list and details.