8.7 Capitation Fees for Plan B (Long-term Care)
General Policy Description
PharmaCare Plan B covers B.C. residents who are permanent residents of long-term care facilities licensed under the Community Care and Assisted Living Act and patients of hospitals licensed under Part 2 of the Hospital Act.
Policy details
Eligible facilities
PharmaCare Plan B covers B.C. residents who are permanent residents of long-term care facilities (excluding extended-care, acute-care, multi-level and assisted living facilities) that are licensed under the Community Care and Assisted Living Act and patients of hospitals licensed under Part 2 of the Hospital Act.
Payment process
Each long-term care facility is served by one contracted pharmacy.
To receive payment for services to a long-term care facility, a pharmacy must be enrolled with PharmaCare in the Plan B pharmacy sub-class. See the PharmaCare Provider Enrolment Guide for more information.
Pharmacies servicing long-term care facilities provide residents with medications packaged in a monitored dosage system.
PharmaCare pays a monthly fee (capitation fee) to pharmacies contracted to provide service to a long-term care facility for each bed occupied by a patient receiving Plan B coverage. See Related Services List for what is included in the capitation fee.
Capitation fee
At the end of each month, PharmaCare pays the contracted pharmacy a capitation fee for each bed that
- The pharmacy has serviced, regardless of the level of service provided, and
- Was occupied by a recipient of PharmaCare Plan B coverage
The capitation fee is $65. The capitation fee is paid in addition to eligible drug costs.
Payments are per serviced bed, regardless of whether different residents have occupied a bed during the month.
Capitation fee payment is based on the actual occupancy of the facility (i.e., the actual number of occupied beds for the month), not on the maximum licensed capacity of the facility.
Capitation fees are not made for short-term (“respite”, “swing”, or “temporary”) patients in a facility. Claims for pharmacy services for respite patients must be made under Fair PharmaCare or Plan C, depending on each patient’s eligibility.
Plan B payments are monitored. Any over-payment in a given month will be recovered. All PharmaCare payments are subject to audit by the Ministry of Health.
All supporting documentation for Plan B invoices (e.g., working papers, prescriptions, authorizations, and the PHN list for which claims were made on the invoice) must be retained on file by the pharmacy in accordance with the Audit Policy.
Relationship to other fees
No dispensing fees or special services fees are paid for Plan B patients. These are covered by the capitation fee.
Pharmacists may charge a fee for administering a publicly funded vaccine to a Plan B patient. For details, see Section 8.10—Pharmacist Administration of Drugs and Vaccines.
Changes in facility licence, licensee or administration
The British Columbia PharmaCare Pharmacy Agreement for the Provision of PharmaCare Services to Long Term Care Facilities is valid only for the licensed facility named in the agreement.
In the event of a change in the facility licence or licensee (e.g., a change in facility name, address, etc.), the pharmacy must
- Obtain a new “Appointment of Pharmacy Services” agreement from the facility; and
- Sign a new British Columbia PharmaCare Pharmacy Agreement for the Provision of PharmaCare Services to Long Term Care Facilities
If there is a change of administration at a long-term care facility, the facility must
- Provide the pharmacy with a new “Appointment of Pharmacy Services” agreement
Procedures for pharmacies
Invoicing
Submit only one invoice per pharmacy per month for Plan B capitation fees (i.e., all contracted care facilities must be claimed on the same invoice). Multiple invoices cannot be processed.
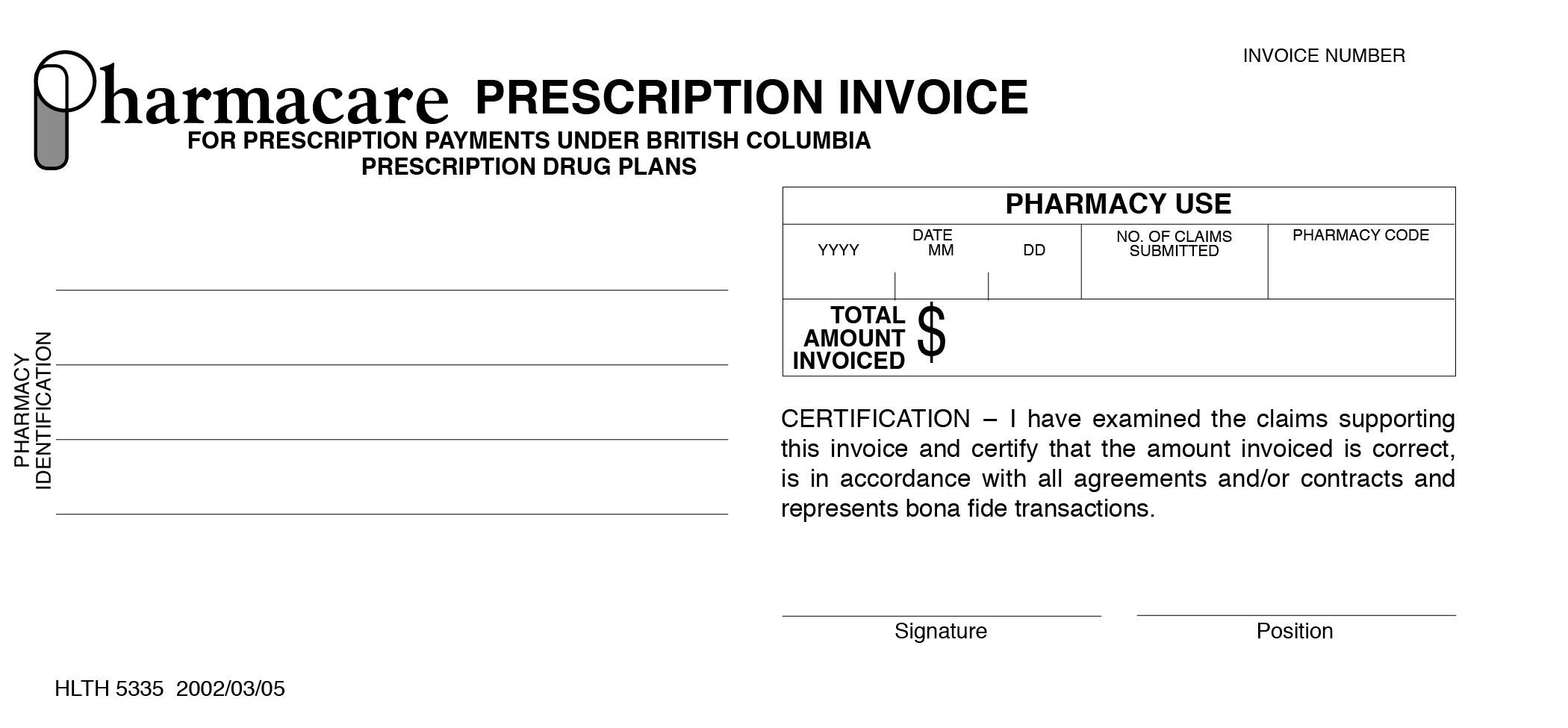
Invoices for Plan B must be submitted on a monthly basis, using PharmaCare Prescription Invoices.
To order additional Invoices, contact the PharmaCare Help Desk.
Submit Plan B monthly invoices to PharmaCare at or near the end of each month. This ensures that the information on the number of occupied and serviced beds for the month is accurate.
To submit an invoice for Plan B
- On a PharmaCare Prescription Invoice, complete the following:
- Pharmacy identification (i.e., name and address of the pharmacy)
- Current date
- Number of claims submitted (i.e., number of claimed beds)
- Pharmacy code
- Total $ amount invoiced
- Write "Nursing Home Beds" at the top of the invoice.
- Write the month to which the invoice applies at the top of the invoice.
This is necessary as the "Current Date" in step 1 does not always reflect the month of service.
- Sign the invoice and include your position in the pharmacy.
Unsigned invoices will be returned by PharmaCare without payment.
- Mail the invoice to the
PharmaCare Help Desk
PO Box 9655 Stn Prov Govt;
Victoria BC V8W 9P2
Tools and resources
For questions about Plan B billings, contact the PharmaCare Help Desk.
To order PharmaCare Prescription Invoices, contact the PharmaCare Help Desk and provide your Site ID.
