Extended health and dental plan for excluded employees
The extended health plan is designed to partially reimburse you for a specific group of medical expenses which are not covered by the Medical Services Plan or the PharmaCare program.
The dental plan is designed to assist you with the cost of your dental care and reimburses most basic and major dental and orthodontic services.
Everyone is unique and has different needs for benefits. There are a number of choices in the Flexible Benefits Program that enable you to create a benefits package to meet your needs.
For each benefit, you’ll either select the option that best meets your needs, or you’ll waive coverage.
The information provided in the guide summarizes the terms and provisions of the health and dental benefits for excluded employees.
In the event of any conflict between the contents of the guide and the actual plans, contracts or regulations, the provisions outlined in those documents apply.
On this page
- Extended health benefits at a glance
- Medical Services Plan
- Extended health plan overview
- Prior authorization and specialty drugs
- Dental benefits at a glance
- Dental plan overview
- Health Spending Account (HSA)
- How to make a claim
Extended health benefits at a glance
The following table summarizes the coverage in each option under the extended health benefits plan. For your convenience, we’ve included annual net pricing information with each table.
If the cost of the option you choose is less than the fully funded option, you’ll have leftover flex credits. The annual price will show a dollar amount credit (for example, $198 CR).
If the cost of the option you choose is $0, this is the fully funded option.
If the cost of the option you choose is greater than the fully funded option, you’ll have to partially pay for that option. The annual price will show a dollar amount cost (for example, $340).
| Extended health plans | Waive | Coordination |
Comprehensive (fully funded) |
Enhanced (2-year lock-in) |
|---|---|---|---|---|
| Annual deductible | No coverage | $100 | $100 | $0 |
| Reimbursement (for most expenses, including prescription drugs) | No coverage | Reimbursed at 20% for the first $5,000 paid in a calendar year per person and then 100% for the balance of the year (subject to some restrictions, reasonable and customary limits and plan maximums) | Reimbursed at 80% for the first $2,000 paid in a calendar year per person and then 100% for the balance of the year (subject to some restrictions, reasonable and customary limits and plan maximums) |
100% |
|
Lifetime maximum |
No coverage |
$3 million (includes coverage for out-of-province or out-of-country medical emergencies) |
$3 million (includes coverage for out-of-province or out-of-country medical emergencies) |
$3 million (includes coverage for out-of-province or out-of-country medical emergencies) |
|
Paramedical services (acupuncture, chiropractor, massage therapy, naturopathic physician, physiotherapy, podiatry) |
No coverage |
All services combined: $500/year/person Reimbursement subject to reasonable and customary limits |
$750/year for massage/person Reimbursement subject to reasonable and customary limits |
$1,000/year for massage/person $1,500/year for physio/person $500/year/other services/person Reimbursement subject to reasonable and customary limits |
| Vision | No coverage | $250/24 months for adults $250/12 months for dependent children |
$400/24 months for adults $300/12 months for dependent children |
$500/24 months for adults $500/12 months for dependent children |
| You | $300 CR | $198 CR | $0 | $340 |
| You plus 1 dependant | $459 | |||
| You plus 2 or more dependants | $578 |
Tips
- To submit eClaims, register and log in to My Canada Life at Work, Canada Life’s plan member website. My Canada Life at Work provides online access to your personalized extended health and dental coverage and claims information
- Claiming deadline for extended health and dental is 15 months from the date the expense was incurred
- Ask your doctor or pharmacist if there’s a less expensive generic medication that's right for you
- Remember to update your benefits coverage as your personal circumstances change
Medical Services Plan
Impact to extended health plan
New or returning to B.C.
- Visit an ICBC office to obtain a BC Services card
- Apply for MSP coverage
It’s recommended that you complete these steps as soon as you arrive in order for the application to be processed and to ensure coverage is not delayed. More information on this process is available on the How to apply page on MSP’s website.
Leaving B.C.
Leaving British Columbia temporarily can impact your continued coverage under MSP. More information related to both temporary and permanent absences from B.C. is available in the Leaving B.C. brochure.
To request MSP account changes (for example: address changes, adding or removing dependants or re-certifying your child as a full-time student) and/or to submit documentation online, please visit the Managing your MSP account page.
Questions
Extended health plan overview
Canada Life administers your extended health plan on behalf of your employer. Detailed descriptions of expenses eligible for reimbursement under this plan are provided in the table below.
There's a lifetime maximum of $3 million per covered person, which includes coverage for out-of-province or out-of-country medical emergencies. If you reach this lifetime maximum because of a serious illness, it may be reinstated based on satisfactory evidence provided by the employee to Canada Life of complete recovery and return to good health.
Reimbursement
Your rate of reimbursement depends on the option you select. Reimbursement is made for eligible expenses which are subject to some restrictions, reasonable and customary limits and plan maximums.
Before purchasing an item or service, it's your responsibility to confirm it’s covered. A claim for an item or service purchased from a provider that is not approved by Canada Life may be declined.
Contact Canada Life if the item is not listed in this guide. It's recommended that you get an expense pre-approved if the cost is over $1,000.
What's covered by your extended health plan
The following is a list of expenses that are eligible for reimbursement under the extended health plan when incurred as a result of a necessary treatment of an illness or injury and, where applicable, when ordered by a physician and/or surgeon. Check My Canada Life at Work for detailed information or contact Canada Life at 1-855-644-0538. The value of your entitlement will be impacted by the option you select.
|
Feature |
Coverage |
|---|---|
|
Accidental injury to teeth |
Dental treatment by a dentist or denturist for the repair or replacement of natural teeth or prosthetics, which is required and performed and completed within 52 weeks after an accidental injury that occurred while covered under this plan. No reimbursement will be made for temporary, duplicate or incomplete procedures, or for correcting unsuccessful procedures. Expenses are limited to the applicable fee guide or schedule. Accidental means the injury was caused by a direct external blow to the mouth or face resulting in immediate damage to the natural teeth or prosthetics and not by an object intentionally or unintentionally being placed in the mouth. |
|
Acupuncture |
Acupuncture treatments performed by a medical doctor or an acupuncturist registered with the College of Traditional Chinese Practitioners and Acupuncturists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. |
|
Braces, prosthetics and supports |
To be eligible for reimbursement, you must include a practitioner’s note for all prosthetics, braces and supports to confirm the medical need for the device. Accepted practitioners include licensed chiropractors, physiotherapists and physicians. The prescription must include the medical condition and the braces must contain rigid material. |
|
Breast prosthetics |
See the 'Mastectomy forms and bras' section of this table for information. |
|
Chiropractor |
Chiropractic treatments performed by a chiropractor registered with the College of Chiropractors of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. X-rays taken by a chiropractor are not eligible for reimbursement. |
|
Contraceptives |
Please contact Canada Life or sign in to My Canada Life at Work and enter the product DIN to confirm if the prescribed contraceptive is covered.
|
|
Counselling |
Out-of-hospital treatment by a registered psychologist, qualified social worker, qualified psychotherapist, qualified therapist or qualified counsellor payable to a maximum of $1,000/year/covered individual. A claim for an item or service purchased from a provider that is not approved by Canada Life may be declined. Contact Canada Life at 1-855-644-0538 to confirm provider eligibility. Visit Careers & MyHR for information about short-term counselling available through the Health and well-being program. |
|
Drugs and medicines |
Covered drugs and medicines purchased from a licensed pharmacy, which are dispensed by a pharmacist, physician or dentist subject to PharmaCare’s policies including reference-based pricing and lowest cost alternative. Drugs and medicines include:
Reimbursement of eligible drugs and medicines will be based on a maximum dispensing fee of $7.60 and a maximum mark-up of 7% over the manufacturer’s list price. All plan members must sign up for PharmaCare to assist with prescription coverage, limiting the impact on your lifetime maximum. Unless medical evidence is provided to Canada Life that indicates why a drug is not to be substituted, Canada Life can limit the covered expense to the cost of the lowest priced interchangeable drug. Prior authorization For more information regarding prior authorization and specialty drug processes, sign in to My Canada Life at Work and click on Info centre > Benefits information sheet or see the 'Prior authorization and specialty drugs' section. No benefits will be paid for:
|
|
Emergency ambulance services |
Emergency transportation by licensed ambulance to the nearest Canadian hospital equipped to provide medical treatment essential to the patient. Air transport when time is critical and the patient’s physical condition prevents the use of another means of transport. Doctor’s note may be required. Emergency transport from one hospital to another only when the original hospital has inadequate facilities. Charges for an attendant when medically necessary. |
|
Examinations: medical |
Medical examinations rendered by a physician, required by a statute or regulation of the provincial and/or federal government for employment purposes, for you and all your registered dependants, provided such charges are not otherwise covered. |
|
Examinations: vision |
Fees for routine eye examinations to a maximum of $100/24 months/person over the age of 19 when performed by a physician or optometrist. Exams for persons under age 19 and over age 64 are covered under the Medical Services Plan. The balance not covered by the Medical Services Plan for individuals over age 64 is eligible for reimbursement under the extended health plan to plan maximum. |
| Gender affirmation |
Gender affirmation coverage with a lifetime maximum of $15,000 per person. Procedures for gender affirmation are covered if the person meets the following conditions:
Submit the form to Canada Life. Canada Life will assess all procedures based on the terms of this plan. Canada Life reserves the right to request details of the procedures performed. Covered gender affirmation procedures include but are not limited to:
Limitations No benefits are paid for:
Contact Canada Life at 1-855-644-0538 or via email through My Canada Life at Work with questions or for additional information. |
|
Hairpieces and wigs |
Hairpieces and wigs, when medically necessary, are eligible for reimbursement to a maximum of $500/24 months. |
|
Hearing aids and repairs |
When prescribed by a physician or audiologist, reimbursements at $1,500/ear/48 months for adults and $1,500/ear/24 months for children. This benefit is not subject to an annual deductible. The prescription must be included with the claim. Batteries, recharging devices or other such accessories are not covered. |
|
Hospital charges |
Additional charges for semi-private or private accommodation over and above the amount paid by provincial health care for a normal daily public ward while you're confined in a hospital under active treatment. This does not include telephone or TV rental or other amenities. |
|
Massage therapy |
Massage treatments performed by a massage practitioner registered with the College of Massage Therapists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. X-rays taken by, and drugs, medicines or supplies recommended and prescribed by a massage therapist are not covered. |
|
Mastectomy forms and bras |
Mastectomy forms and bras are eligible for reimbursement to a maximum of $1,000/12 months. |
|
Medical aids and supplies |
A variety of medical aids and supplies as follows: For diabetes:
NOTE: To be eligible for Continuous Glucose Monitor (CGM) or Flash Glucose Monitor (FGM) coverage, you must first apply for coverage through BC PharmaCare Special Authority. Portions of the cost that are not paid by BC PharmaCare, such as the deductible and the coinsurance amount, can be claimed under the extended health plan.
NOTE: If you switch from using testing supplies to an insulin injector, testing supplies are not covered for the next 60 consecutive month period. Other medical aids and supplies:
Standard durable equipment as follows: The cost of renting, where more economical, or the purchase cost of durable equipment for therapeutic treatment including:
Pre-authorization is recommended for items costing over $1,000 and is required for items over $5,000. |
|
Naturopathic physician |
Naturopathic services performed by a naturopathic physician licensed by College of Naturopathic Physicians of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. X-rays taken, and drugs, medicines or supplies recommended and prescribed by a naturopathic physician are not covered. |
|
Needleless injectors |
When prescribed by a physician:
|
|
Orthotics and orthopedic shoes |
When prescribed by a physician or podiatrist when medically necessary, custom-fit orthotics or orthopedic shoes, including repairs, orthotic devices and modifications to stock item footwear but not including arch supports/inserts. Payable to a maximum of $400/person/calendar year. Not all casting techniques are approved for coverage, so please confirm with Canada Life prior to purchase. Custom-made orthotics When submitting claims for custom-made orthotics, include the following information:
Custom-made orthopedic shoes When submitting claims for custom-made orthopedic shoes, include the following information:
Please review the Canada Life Benefit information sheet on My Canada Life at Work > Info centre for more information about claiming orthotics and orthopedic shoes. |
|
Out-of-province/out-of-country emergencies |
Reasonable charges for a physician’s services due to an emergency are eligible for reimbursement, less any amount paid or payable by the Medical Services Plan, subject to the lifetime maximum of $3 million for extended health and out-of-province/out-of-country emergencies. |
|
Paramedical services |
Services provided by licensed paramedical practitioners. For the purposes of this plan, paramedical services are a defined group of services and professions that supplement and support medical work, but do not require a fully qualified physician. These services include:
Paramedical services are subject to reasonable and customary (R&C) limits until the annual maximum is reached. R&C represents the standard fees healthcare practitioners would charge for a given service. They're reviewed regularly and are subject to change at any time. If your healthcare practitioner charges more than a R&C limit, you'll be responsible for paying the difference. For R&C charges, log into My Canada Life at Work, go to Benefits > Coverage and balances > Health, Drugs, Vision & Dental (50088) > Health > Health professionals and click on a health professional. If you have any questions about R&C limits for a given service, contact Canada Life at 1-855-644-0538. |
|
Physiotherapist |
Professional services performed by a physiotherapist registered with the College of Physical Therapists of British Columbia. See the 'Paramedical services' section of this table for information about reasonable and customary limits. |
|
Podiatrist |
Professional services performed by a podiatrist registered with the British Columbia Association of Podiatrists. See the 'Paramedical services' section of this table for information about reasonable and customary limits. X-rays taken or other special fees charged by a podiatrist are not covered. |
|
Prostate-serum antigen test |
Once per calendar year. |
|
Smoking cessation products |
Drugs and supplies for prescriptions and non-prescription smoking cessation. Maximum: $300/year/person to a lifetime maximum of $1,000. You must register with the Quittin’ Time Program prior to purchasing any products.
|
|
Vision care |
This benefit is not subject to the deductible and is reimbursed at 100% (to plan limits). Purchase and/or repair of corrective eyewear, charges for contact lens fittings and laser eye surgery, when prescribed or performed by an optometrist, ophthalmologist or physician. Corrective eyewear includes lenses, frames, contact lenses, prescription sunglasses, prescription safety goggles, and vision care repairs. Charges for non-prescription eyewear are not covered. Check My Canada Life at Work to verify your personal eligibility period as coverage for vision care is determined using a rolling eligibility date. Eye exams are a separate feature. See the 'Examinations: visions' section of this table for information about eye exams. No benefits will be paid for vision care services and supplies required by an employer as a condition of employment. |
Any item not specifically listed as being covered under this plan is not an eligible item under this extended health plan.
Extended health general exclusions
No benefits will be paid for:
- Expenses that private benefit plans are not permitted to cover by law
- Services or supplies for which a charge is made only because the person has coverage under a private benefit plan
- The portion of the expense for service or supplies that is payable by the government health plan in the person’s home province, whether or not the person is actually covered under the government health plan
- Any portion of services or supplies which the person is entitled to receive or for which they are entitled to a benefit or reimbursement by law or under a plan that is legislated, funded or administered in whole or in part by a government plan without regard to whether coverage would have otherwise been available under this plan
- Services or supplies that do not represent reasonable treatment
- Services or supplies associated with treatment performed for cosmetic purposes only
- Services or supplies associated with recreation or sports rather than with other regular daily living activities
- Services or supplies associated with the diagnosis or treatment of infertility or contraception except as may be provided under the prescription drug provision
- Services or supplies associated with a covered service or supply unless specifically listed as a covered service or supply, or determined by the plan administrator to be a covered service or supply
- Extra medical supplies that function as spares or alternatives
- Services or supplies received outside Canada except as provided under the out-of-country care provision
- Services or supplies received out-of-province in Canada, unless:
- The person is covered by the government health plan in their home province, or the government coverage replacement plan sponsored by the employer, and
- This plan would have paid benefits for the same services or supplies if they were received in the person’s home province
- Medical evacuation services covered under the employer’s global medical assistance plan
- Expenses arising from war, insurrection or voluntary participation in a riot
- Hospital care for conditions where significant improvement or deterioration is unlikely within the next 12 months. This is considered chronic care
Your extended health plan options
No coverage
If you waive extended health coverage under the Flexible Benefits Program, you'll receive flex credits to use elsewhere.
All employees, regardless of family status, will receive the same number of flex credits upon waiving a benefit plan.
This option has no travel medical emergency coverage.
Coordination
This is a low-cost option which provides a low level of coverage for most services.
This option has a deductible.
This option may work well if you're able to coordinate your benefits with your spouse’s plan, depending on terms of their plan.
If you're coordinating benefits with your spouse and you select this option, your reimbursements under this option (like when you go to the pharmacy) will be the lower portion (that is, 20%). The more significant portion will be reimbursed through your spouse’s plan, after you've submitted a claim to that plan. It’s important to be aware of this so there are no surprises when you're paying for products and services.
You have business and personal travel medical emergency coverage included in the extended health lifetime maximum of up to $3 million.
Comprehensive
This option provides a comprehensive level of coverage in all identified areas (for example: prescription drugs, vision care, paramedical services and medical equipment) and is the fully funded option. This option has a deductible. You have business and personal travel medical emergency coverage included in the extended health lifetime maximum of up to $3 million.
Enhanced
This option has no deductible and a higher reimbursement rate than the other options.
It includes higher coverage for:
- Vision care
- Massage therapy
- Physiotherapy
You have business and personal travel medical emergency coverage included in the extended health lifetime maximum of up to $3 million.
This option has a 2-year lock-in so if you choose it, you must remain under this option for 2 plan years.
Details to consider
- Given your claims history and any anticipated future medical expenses, which option offers the best value? Reviewing your past claims information can help you with anticipating future expenses
- If you're covering dependants, which dependants will you cover? Given their claims history, which option offers the best value for you?
- If you're able to coordinate benefits with a spouse, which option offers the best value to you?
Out-of-province/out-of-country emergency coverage under the extended health group plan
If you’re covered under the Provincial Government Medical Service Plan and the extended health plan (meaning you have not waived coverage), you’re covered for medical emergencies while traveling outside your province or outside Canada, whether for work or personal reasons.
You’re covered for medical emergencies, including those caused by pre-existing conditions (except for a few exclusions) up to the lifetime maximum of $3 million per person.
Your spouse and/or dependants covered under the Provincial Government Medical Service Plan and your extended health group plan are also covered for emergency medical care while travelling for pleasure.
Eligible emergency medical expenses will be reimbursed at 100%, after the annual deductible has been satisfied, and up to plan limits.
Eligible emergency out-of-province/out-of-country expenses
- Local ambulance services when immediate transportation is required to the nearest hospital equipped to provide the treatment essential to the patient
- The hospital room charges and charges for services and supplies when confined as a patient or treated in a hospital. Members should contact Travel Assistance for assistance if they have a medical emergency. Refer to the Travel Assistance Brochure (PDF, 2MB) for contact information. When the patient’s medical condition permits, they'll be returned to Canada. Canada Life's standard out-of-country confinement is up to a semi-private ward rate
- Physician, laboratory and x-ray services
- Prescription drugs
- Other emergency services and/or supplies, if Canada Life would have covered the expenses in your province/territory of residence
- Medical supplies provided during a covered hospital confinement
- Paramedical services provided during a covered hospital confinement
- Medical supplies provided out of hospital if you would have been covered in Canada
- Out of hospital services of a professional nurse
- A sudden and unexpected injury
- The onset of a condition not previously known or identified prior to departure from B.C. or Canada
- An unexpected episode of a condition known or identified prior to departure from B.C. or Canada
An unexpected episode means it would not have been reasonable to expect the episode to occur while travelling outside of Canada. If a person was suffering from symptoms before leaving Canada, Canada Life may request medical documentation to determine whether, in the circumstances, it could have reasonably been anticipated that the person may require treatment while outside Canada.
Non-emergency continuing care, testing, treatment, surgery and amounts covered by any government plan and/or any other provider of health coverage are not eligible.
Exclusions
- Expenses incurred due to elective treatment and/or diagnostic procedures
- Complications related to such treatment expenses incurred due to therapeutic abortion, childbirth, or complications of pregnancy occurring at week 35 or later, or if high risk, during pregnancy
- Charges for continuous or routine medical care normally covered by the government plan in your province/territory of residence
Business travel medical insurance
If you don’t have extended health coverage through your BC Public Service job, you’re not covered by the group business travel insurance plan, except in limited cases.
Before making travel plans, check your travel medical insurance status. If you need to travel for work and you’re not covered by the corporate travel medical policy, you should purchase an individual travel insurance plan and claim the expense through your travel claim.
When purchasing travel insurance, make sure to read and understand the fine print. Most individual travel insurance plans don’t cover pre-existing conditions. Carefully consider your personal health circumstances before agreeing to travel for work.
Optional medical travel insurance
Canada Life has a travel insurance website to enable you to purchase optional travel medical insurance. For more information, review Canada Life’s Optional Emergency Travel Medical Benefit Information Sheet (PDF, 141KB). This travel medical insurance is first payer to your group plan with Canada Life, and you’ll save 10% by purchasing it from this website.
If you have other similar coverage, such as through a credit card plan or another group or individual insurance plan, claims will be coordinated within guidelines for out-of-province/out-of-country coverage issued by the Canadian Life and Health Insurance Association.
To apply, you'll need your Canada Life group plan number (50088) and your identification number from your Canada Life ID card.
This travel insurance has a maximum amount payable per covered trip of $2 million Canadian. Single or annual travel policies are available if you're under 80. There are exclusions for pre-existing conditions.
Travel Assistance
Canada Life's Travel Assistance provides assistance if you or an eligible dependant experiences a medical emergency while traveling out-of-province/out-of-country. Trained personnel who speak various languages will provide advice and coordinate services for you.
This service is available 24 hours a day, 365 days a year and assists members in locating hospitals, clinics and physicians. Travel Assistance also provides the following services:
- Medical advisers
- Advance payment when required for hospital admission
- Helping to locate qualified legal assistance, local interpreters and appropriate services for replacing lost passports
- Assisting unattended children
- Return of vehicle
- Transportation reimbursement
- Medical evacuation
- Travelling companion expenses
- Transportation of remains if a plan member dies while travelling. Expenses for preparing and transporting the plan member’s remains home are covered. The Travel Assistance company can also help make the appropriate arrangements
Travel Assistance provides advice and coordinates services at no additional charge. However, it's not a means of paying for any healthcare expenses that you may require.
The actual cost for any service(s) received is your responsibility. Some of these expenses may be claimed through:
- Medical Services Plan of B.C.
- Travel insurance purchased by you
- Your extended health plan
Please ensure that you have the Travel Assistance phone numbers with you when you travel.
Canada Life has simplified the phone numbers, and you will just require the following 2 phone numbers:
- Canada or U.S.: 1-855-222-4051
- All other locations: 1-204-946-2577
You can find these phone numbers, as well as your plan and personal ID numbers, on your digital benefits ID card available through My Canada Life at Work. Be sure to have access to those numbers and your provincial health care number when you travel for personal identification.
See the Travel Assistance page for more information.
Out-of-country non-emergency coverage
When you receive non-emergency services and supplies while outside of Canada, they are covered if:
- The same services and supplies would have been covered if you received them in Canada
- They meet the same requirements for deductibles, maximums, reimbursements and plan limits
Covered services and supplies include:
- Ambulance services
- Prescription drugs
- Medical supplies
- Paramedical services
- Vision care
- Dental accident treatment
Prior authorization and specialty drugs
Canada Life’s prior authorization process provides an effective approach to managing claims for specific prescription drugs.
How prior authorization works
Prior authorization requires that you request approval from Canada Life for coverage of certain prescription drugs. When a claim is submitted for any of these drugs, they’ll ask for information to help them assess the claim. Your request must be approved before your claim is paid. To ensure your claim is processed without delay, please provide all necessary information before filling a prescription.
Why we require prior authorization
Drugs approved for one or more medical conditions are sometimes prescribed for other conditions without being proven as an effective treatment. The practice of requesting additional information is designed to help:
- Provide coverage for appropriate drug treatment
- Ensure the drugs prescribed are considered reasonable treatment for the condition
- Keep your drug plan affordable and accessible
Drugs requiring prior authorization
Canada Life maintains a limited prior authorization drug list with corresponding forms.
Before approving a claim for any of these drugs, they review the circumstances to determine whether the drug is a reasonable treatment for the condition it was prescribed for.
The prior authorization drug form list does change. Your group benefits plan may not provide coverage for all the prior authorization drugs listed, as coverage depends on the terms of your plan.
To view the prior authorization drug form list, sign in to My Canada Life at Work > Info centre > Forms > Prior authorizations forms to determine which drug requires prior authorization.
If you have questions about which drugs are covered by your plan, call Canada Life's Group Customer Contact Services Office at 1-855-644-0538.
How to request prior authorization
If you’re prescribed a drug that requires prior authorization, you must:
- Fill out the appropriate section(s) of the drug-specific prior authorization form with your doctor
- Submit the form to Canada Life
Your claim can't be considered for reimbursement until they receive this form.
If you anticipate submitting a claim for a drug that requires prior authorization, take the appropriate prior authorization form to your doctor’s appointment.
Completed forms can be emailed, faxed or mailed to Canada Life:
Email
cldrug.services@canadalife.com
Fax
Canada Life
Fax: 1-204-946-7664
Attention: Drug Claims Management
Mail
Canada Life
Attention: Drug Claims Management
Drug Services PO Box 6000
Winnipeg MB R3C 3A5
If your claim is approved, in most cases, additional prior authorization forms for the drug will not be required.
Future claims for the drug will be processed in the same manner as prescription drugs that do not require prior authorization.
Certain drugs may require additional approval after a specified period. In these situations, you may be asked to provide further information regarding the progress of your treatment.
All requests for prior authorization are reviewed by Canada Life. Their decision is based on the information provided to determine whether the prescribed drug represents reasonable treatment.
Notification regarding the claim decision
Once Canada Life reviews your completed prior authorization form, they’ll provide a decision by letter. If the request is declined, you may wish to discuss your medication needs with your doctor or pharmacist. You have the option of paying for the total cost of the drug yourself.
Specialty drug program
Canada Life’s enhanced drug coordination process coordinates eligible drugs under specific provincial programs. You may be required to apply to the provincial program for drug coverage. Some drugs included in this program are also under prior authorization.
How the specialty drug program works
Go to your pharmacy to fill a prescription.
1. The drug is included in the specialty drug program:
- The claim will be paid, but you’ll need to apply to your provincial program
- You’ll receive a letter to apply to the provincial program and respond to Canada Life within 70 days
- Canada Life will coordinate your drug plan with your provincial plan
OR
2. The drug is included in the specialty drug program and the prior authorization program:
- If your claim is denied, you’ll receive a letter to apply to your provincial program
- If approved, Canada Life will pay any amounts not eligible under the provincial program
- If the provincial plan declines your claim, send the prior authorization form to Canada Life to assess eligibility under the drug plan
- You’ll be notified if your claim is accepted or not
Prescription drug coverage: BC Public Service extended health plan
The following information provides details of the prescription drug coverage under the extended health plan for BC Public Service employees.
What is BC PharmaCare and how does it coordinate with your drug plan?
BC PharmaCare helps all B.C. residents with the cost of eligible prescription drugs, even if you have private drug coverage through the BC Public Service extended health plan. Here’s how it works:
- BC PharmaCare starts paying after your total prescription costs reach your annual deductible
- Your deductible is based on 3% of your net family income
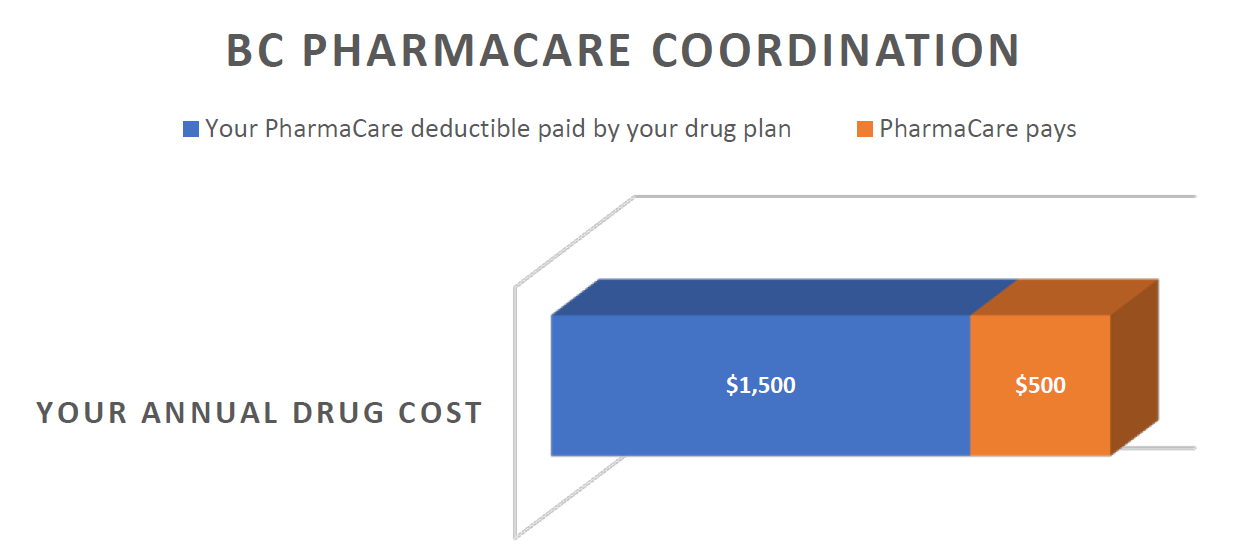
- Until you reach your deductible, your extended health plan will pay in accordance with the plan’s reimbursement limits. In the example pictured below, based on a net family income of $50,000 and total eligible family drug costs of $2,000 for the year, BC PharmaCare will start paying after your family’s eligible drug costs have reached $1,500 ($50,000 x 3%) within a calendar year.
How does PharmaCare know how to calculate my deductible?
You must register for Fair PharmaCare for BC PharmaCare to access your income tax returns to calculate your deductible.
If you do not register, your deductible will be set at the maximum of $10,000, which will add unnecessary costs to your drug plan.
What if I haven't registered with Fair PharmaCare?
If the eligible drug costs for you and your dependant(s) reach a certain amount in a calendar year, Canada Life will notify you to register for Fair PharmaCare or your drug claims will be temporarily suspended until Canada Life gets confirmation that you’ve registered. Learn more about Fair PharmaCare.
In addition to coordinating drug costs with BC PharmaCare, the drug plan for BC Public Service employees follows BC PharmaCare’s pricing policies which include the Low Cost Alternative (LCA) Program and the Reference Drug Program (RDP).
What’s the Low-Cost Alternative (LCA) Program?
When the same drug is made and sold by more than one manufacturer, the plan covers the less costly version. Drugs deemed the 'lowest cost alternative' are usually (but not always) generics. The LCA drugs (usually generics) are fully covered by the plan, but the more costly brand name drugs are only partially covered up to the LCA price.
For example:
- Celexa™ is the brand name version of a popular antidepressant
- The cost of one Celexa 20mg tablet = $1.7046 (partially covered)
- The generic version of one Celexa 20mg tablet = $0.14 (fully covered)
Your drug plan would only pay up to the cost of the generic version ($0.14) if you filled a prescription for Celexa™, subject to the terms of your group benefits plan. To get fully reimbursed, you would need to purchase the generic version which can be done by the pharmacist without authorization from your doctor.
If there’s a medical reason that requires you to take the brand name drug, ask your physician to complete a Request for Brand Name Drug Coverage form (available on the Canada Life website) to provide the medical information why you require the brand name drug.
What’s the Reference Drug Program (RDP)?
Sometimes there are several drugs that treat the same illness or condition that are very similar in effectiveness, chemical structure and safety.
There are 7 therapeutic categories in the Reference Drug Program.
- Angiotensin receptor blockers for high blood pressure
- Proton pump inhibitors for acid reflux and ulcers
- Statins for high cholesterol
- H2 blockers for acid reflux
- Calcium channel blockers for high blood pressure
- Angiotensin converting enzyme inhibitors for high blood pressure
- Non-steroidal anti-inflammatories for pain and inflammation
PharmaCare reviews the cost of the drugs within each category and determines the maximum daily cost it will cover.
Each therapeutic category has reference drugs which are the most cost effective. These are fully covered by the plan, in accordance with the plan’s reimbursement formula. However, the more expensive drugs within a therapeutic category are considered non-reference drugs and these will only be partially covered, up to the maximum daily price.
For example, let’s take the statins, a popular class of drugs for high cholesterol:
- Reference statin drugs: atorvastatin and rosuvastatin are fully covered
- Non-reference statin drugs: fluvastatin, lovastatin, pravastatin, simvastatin are only reimbursed to a daily maximum of $1.71
Can I get fully reimbursed for a non-reference drug within the Reference Drug Program if my doctor thinks it’s medically necessary?
If your doctor thinks that it’s medically necessary for you to take a non-reference drug because you’ve already tried a reference drug and it hasn't been effective, you may ask your doctor to apply to BC PharmaCare’s Special Authority Program on your behalf.
Once approved, you can send in the form to Canada Life to get a pricing exception and full coverage, to plan limits, for your non-reference RDP drug.
For any additional information regarding the Reference Drug Program, please refer to the PharmaCare website.
What if I am already at the pharmacy and realize that my doctor prescribed a non-reference drug? What can I do to get the drug changed to a fully covered drug?
You can go back to your doctor and ask them to prescribe a reference drug within that therapeutic category or ask your pharmacist if they can adapt the prescription to a reference drug.
Under very limited conditions, pharmacists in British Columbia can change certain prescriptions from one drug to another without consulting your doctor.
BC PharmaCare’s Special Authority drugs
In addition, some drugs may be eligible for coordination with BC PharmaCare’s Special Authority (SA) program.
If you’re claiming a drug included in the SA Program, you may be eligible for coverage under the government plan.
Your pharmacy will submit your claim to the provincial program and if approved, the decision will be automatically shared with Canada Life.
If you are declined by the provincial program, a copy of the BCSA application form with the provincial decline included on the form can be sent to Canada Life at:
Canada Life Drug Claims Management
Email
cldrug.services@canadalife.com
Mail
PO Box 6000
Winnipeg MB R3C 3A5
Fax
1-204-946-7664
Dental benefits at a glance
The following table summarizes the coverage in each option under the dental benefits plan. For your convenience, we’ve included annual net pricing information with each table.
If the cost of the option you choose is less than the fully funded option, you’ll have leftover flex credits. The annual price will show a dollar amount credit (for example, $195 CR).
If the cost of the option you choose is $0, this is the fully funded option.
If the cost of the option you choose is greater than the fully funded option, you’ll have to partially pay for that option. The annual price will show a dollar amount cost (for example, $213).
|
Dental plan |
Waive |
Coordination |
Comprehensive (fully funded) |
Enhanced (2-year lock-in) |
|---|---|---|---|---|
|
Basic |
No dental coverage |
20% recall for adults: 9 months |
100% recall for adults: 9 months |
100% recall for adults and children: 6 months |
|
Major |
No dental coverage |
50% |
65% |
85% |
|
Orthodontic (LTM = lifetime maximum) |
No dental coverage |
50% with LTM of $2,000 |
55% with LTM of $3,500 |
55% with LTM of $5,000 |
|
You |
$300 CR |
$195 CR |
$0 |
$213 |
|
You plus 1 dependant |
$300 CR | $195 CR | $0 |
$426 |
|
You plus 2 or more dependants |
$300 CR | $195 CR | $0 |
$633 |
Tips
- To submit eClaims, register and log in to My Canada Life at Work, Canada Life’s plan member website. My Canada Life at Work provides online access to your personalized extended health and dental coverage and claims information
- Claiming deadline for extended health and dental is 15 months from the date the expense was incurred
- Remember to update your benefits coverage as your personal circumstances change
Dental plan overview
Canada Life administers your dental plan on behalf of your employer. Dental coverage is available for:
- Services in B.C.
- Emergency dental services while traveling outside of B.C. up to the amount your plan would have covered if the services had been performed in B.C.
What's covered by your dental plan?
Dental services fall into 3 categories:
- Basic preventative and restorative services
- Major services
- Orthodontic services
Reimbursement
Your rate of reimbursement depends on the option you select.
Dentists set their own rates for service, but reimbursement of dental fees under this group plan is subject to the dental fee schedule published by the BC Dental Association for dentists, dental specialists and denturists to plan limits.
You're responsible for any fees that exceed reasonable and customary and plan limits. Always ask for pre-approval.
If services are performed by a specialist, the fee is equal to that of the general practitioner, plus 10%.
It's your responsibility to verify that an item or service is covered prior to treatment. A claim for a service or supply that was purchased from a provider that is not approved by Canada Life may be declined. Contact Canada Life if the item is not listed in this guide.
Basic services
Basic dentistry comprised of routine services available in the office of a general practicing dentist and are necessary to restore teeth to natural or normal function.
Diagnostic services
Procedures conducted to determine or diagnose the dental treatment required, including:
- Standard oral examinations
- Specific oral examinations
- X-rays (including panoramic X-rays once every 5 years)
- A specific oral exam will be reimbursed once for any specific area and only if a standard oral examination hasn't been reimbursed within the previous 60 days
- A complete oral exam will be reimbursed once every 3 years, but not if the plan has not reimbursed for any examination during the preceding 9 months
Preventative services
Procedures that prevent oral diseases, including:
- Cleaning and polishing teeth
- Scaling
- Topical fluoride: once every 9 months
- Pit and fissure sealants, preventative restorative resins
- Fixed space maintainers intended to maintain space and regain lost space, but not to obtain more space
Restorative services
- Fillings: amalgam fillings and composite (white) fillings on all teeth. Specialty fillings and crowns such as synthetic porcelain, plastic, composite resin, stainless steel and gold may result in additional cost to be paid by the employee or dependant
- Stainless steel crowns on primary and permanent teeth
- Inlays and onlays
Only one inlay, onlay or other major restorative service involving the same tooth will be covered in a 5-year period.
Surgical services
All necessary procedures for extractions and other surgical procedures necessary for the treatment of disease of the soft tissue (gum) and the bones surrounding and supporting the teeth.
Endodontics
Treatment of diseases of the pulp chamber and pulp canal, including but not limited to basic root canal.
Periodontal services
Treatment of diseases of the soft tissue (gum) and bones surrounding and supporting the teeth, including occlusal adjustment, root planing, gingival curettage and scaling.
Replacements and repairs
- The repair of fixed appliances and the rebase or reline of removable appliances (may be done by a dentist or by a licensed dental mechanic). Relines will only be covered once per 24-month period
- With crowns, restoration for wear, acid erosion, vertical dimension and/or restoring occlusion is not covered. Check with Canada Life before proceeding
- Temporary procedures (for example: while awaiting repair of an appliance) are not covered
Recall check-up schedule
For dependent children under 19 years of age, general recall services (oral exam, polishing, scaling, and fluoride) are covered once every 6 calendar months.
For adults and students covered under the dental plan, age 19 and older, these services are covered once every 9 calendar months under the Coordination and Comprehensive option, and 6 calendar months if you’re under the Enhanced option.
Major services
Major services apply to services required for reconstruction of teeth and for the replacement of missing teeth (for example: crowns, bridges and dentures), where basic restorative methods cannot be used satisfactorily. To determine how much of the cost will be paid by the plan, and the extent of your financial liability, you should submit a treatment plan to Canada Life for approval before treatment begins.
Only one major restorative service involving the same tooth will be covered in a 5-year period.
Restorative services
- Veneers
- Crowns and related services
- Specialty crowns and fillings, such as synthetic porcelain plastic, composite resin, stainless steel and gold may result in additional cost to be paid by the employee or dependant
Fixed prosthetics
Bridgework to artificially replace missing teeth with a fixed prosthesis.
Removable prosthetics
- Full upper and lower dentures or partial dentures of basic standard design and material
- Full dentures can be provided by a dentist or a licensed dental mechanic
- Partials can only be provided by a dentist
No benefit is payable for the replacement of lost, broken or stolen dentures.
Broken dentures, however, can be repaired under basic services.
Replacement and repairs
Removal, repairs and re-cementation of fixed appliances.
Plan limits
A dentist may charge more for services than the amount set in the governing schedule of fees or may offer to provide services more frequently than provided for in the fee guide.
You're responsible for any financial liability resulting from services performed which are not covered, or that exceed the costs covered by the plan.
Orthodontic services
This plan is designed to cover orthodontic services provided to maintain, restore or establish a functional alignment of the upper and lower teeth. The plan will reimburse orthodontic services performed after the date coverage begins.
Pre-approval
To claim orthodontic benefits, Canada Life must receive a treatment plan (completed by the dentist or orthodontist) before treatment starts.
Reimbursement
The carrier will pay benefits monthly.
Photocopies of receipts, as treatment progresses, must be submitted monthly (do not hold receipts until the treatment is complete).
You can submit monthly claims through My Canada Life at Work.
If you pay the full amount to the dentist in advance of completed treatment, the carrier will prorate benefit payment over the months of the treatment period.
No benefit is payable for the replacement of appliances which are lost or stolen.
Treatment performed solely for splinting is not covered.
Dental general limitations
No benefits will be paid for:
- Expenses that private benefit plans are not permitted to cover by law
- Services and supplies the person is entitled to without charge by law or for which a charge is made only because the person has coverage under a private benefit plan
- Services or supplies that do not represent reasonable treatment
- Services or supplies associated with treatment performed for cosmetic purposes only
- Services or supplies associated with congenital defects or developmental malformations in people 19 years of age or over, except orthodontics
- Services or supplies associated with temporomandibular joint (TMJ) disorders
- Services or supplies associated with vertical dimension correction
- Services or supplies associated with myofascial pain
- Expenses arising from war, insurrection or voluntary participation in a riot
- Services or supplies covered under this plan’s healthcare benefit, unless the amount payable for the same expense is greater under this benefit provision
Any other item not specifically listed as being covered under this plan is not an eligible item under this dental plan.
Your dental plan options
Waive
If you waive dental plan coverage under the Flexible Benefits Program, you’ll receive additional flex credits to use elsewhere.
All employees, regardless of family status, will receive the same number of flex credits upon waiving a benefits plan.
Coordination
This is a low-cost option with a lower level of dental coverage.
This option may work well if you're able to coordinate your benefits with your spouse’s plan, depending on the terms of their plan.
This option reimburses:
- Basic services at 20%
- Major services at 50%
- Orthodontic services at 50% (with a lifetime maximum of $2,000 per person)
The recall schedule is every 9 months for adults and every 6 months for children.
If you’re coordinating benefits with your spouse and you select this option, your reimbursement will be the lower portion. The more significant portion will be reimbursed through your spouse’s plan after you’ve submitted a claim to that plan.
Comprehensive
This option provides a comprehensive level of dental coverage.
It reimburses:
- Basic services at 100%
- Major services at 65%
- Orthodontic services at 55% (with a lifetime maximum of $3,500 per person)
This is the fully funded option.
The recall schedule is every 9 months for adults and every 6 months for children.
Enhanced
This option provides an enhanced level of coverage.
It reimburses:
- Basic services at 100%
- Major services at 85%
- Orthodontic services at 55% (with a lifetime maximum of $5,000 per person)
The recall schedule is every 6 months for adults and children.
This option has a 2-year lock-in, so if you choose it, you must remain under this option for 2 plan years.
Details to consider
- If you’re covering dependants, which dependants will you cover?
- Which features of the dental plan are most important to you and your dependants (for example: basic services, major services, orthodontics)?
- If you’re able to coordinate benefits with a spouse, which option offers the best value to you?
Health Spending Account (HSA)
A Health Spending Account (HSA) allows you to set aside some of your flex credits to pay for eligible out-of-pocket expenses that are not covered by your extended health and dental plans.
| Health Spending Account (HSA) |
Waive |
Elect |
|---|---|---|
| You can only allocate funds to your HSA during initial enrolment or Open Enrolment |
No HSA |
Minimum: $100 Maximum: Please use the 2026 Flexible Benefits Calculator Tool (XLSM, 61KB) to confirm your maximum prior to enrolling. Individual maximum may vary |
How it works
During your initial enrolment and every year during the Open Enrolment period, you decide whether to establish a Health Spending Account (HSA) and choose how many flex credits to allocate to it. During the plan year, when you have out-of-pocket expenses for eligible items or services, you can claim them against funds in your HSA.
The order in which you allocate your flex credits is important and depends on tax status of the benefits you choose.
First, you use your flex credits for your non-taxable benefits, which are your extended health and dental plans. Next, you can allocate your remaining flex credits to a Health Spending Account (minimum $100).
Any flex credits you don't use are added to your salary. These are taxed and then used to pay for your taxable benefits (Employee Basic Life Insurance) and any optional insurance products you chose.
- If you put flex credits into a Health Spending Account, you can only access that money to get reimbursed for eligible expenses. You can't take the money out as cash
- Funds in a Health Spending Account must be claimed within 2 plan years, or you lose them (see the 'Use it or lose it' example below)
- If your employment ends, you cannot claim expenses incurred after your termination date. Any unused funds will be forfeited
- The claiming deadline for your Health Spending Account is February 28 following the year in which the expense was incurred
- You can claim funds from your Health Spending Account after submitting your claim to your extended health or dental plan and your spouse’s plan, if applicable
- Unless you have coordinated benefits with your spouse, you can claim funds from your Health Spending Account when you submit your initial claim for reimbursement. Just include your Health Spending Account information on the electronic or paper claim. Check My Canada Life at Work for your Health Spending Account balance
- To get reimbursed from your Health Spending Account, the item or service must qualify as a medical expense under the Canada Revenue Agency income tax guideline
Example: use it or lose It
Greg put $200 flex credits into his Health Spending Account for plan year 2020. Greg can claim funds against eligible out-of-pocket expenses incurred throughout 2020, up to and including December 31, 2021. Canada Life must receive claims by February 28 following the year in which the expense was incurred.
It’s recommended that you submit claims immediately after treatment. Late claims will not be accepted by Canada Life.
The list of eligible expenses and dependent family members follows the Canada Revenue Agency income tax guidelines. These guidelines cover more items than your benefits plan, so you may be able to claim more items through your Health Spending Account.
Details to consider
Review your previous claims history and try to determine if you have upcoming expenses (for example: new glasses). Given this information, are you likely to have out-of-pocket expenses? Is it worthwhile to you considering the risk involved and the extra effort required?
If you conclude that you’d like to allocate some flex credits to a Health Spending Account, what allocation will work best for you? Remember, you cannot cash in your Health Spending Account, so choose an amount that you know you’ll be able to claim.
Your Health Spending Account options
Waive
No flex credits will be allocated to a Health Spending Account. Any leftover flex credits will be paid out as taxable cash.
Elect a Health Spending Account
Flex credits are allocated to a Health Spending Account in your name to be used for reimbursement of eligible expenses. The minimum is $100; the maximum is the flex credits left over after paying for your extended health and dental coverage.
Any leftover flex credits that are not allocated to a Health Spending Account will be paid out as taxable cash.
How to make a claim
This section provides you with methods to make an extended health, drug or dental claim.
My Canada Life at Work
My Canada Life at Work is Canada Life's self-service website for your extended health and dental plans. On this website, you can:
- Submit eClaims
- Update direct deposit banking information
- View your coverage at a glance
- Track your eligibility and limits
- View or print ID cards
Benefit ID cards are no longer being mailed to plan members but rather can be accessed online through My Canada Life at Work.
Once your benefits are active, log into Employee Self Service (ESS) to view your Canada Life Policy (50088) and ID number.
- Time and Pay: access from work (IDIR restricted)
- Time and Pay: access from home (IDIR restricted)
Time and Pay > Employee Self Service > Benefits Summary > Dental Flex or Extended Health Flex
You will need the policy number and ID numbers to register for access to My Canada Life at Work for Plan Members.
Please allow 3 to 5 business days after your benefits are in effect to register. You can also download the My Canada Life at Work Mobile app to your devices.
If you have problems registering with My Canada Life at Work, please call Canada Life.
Most claims can be submitted online, but there are still some claims that require members to complete a specific claim form. These claim forms and receipts can be uploaded on My Canada Life at Work so members do not have to mail them to Canada Life.
Members can upload a photocopy, scan or picture of their claims by logging into My Canada Life at Work and going to Make a claim > Start a claim > Who is the claim for? > Select a plan for this claim.
Plan types:
Health, Drugs, Vision & Dental (50088):
- Health professionals (massage, chiropractor etc.)
- Medical equipment and supplies (orthotics, prosthetics etc)
- Vision Care
- Drugs
- Dental
- Ambulance services
- Out of Country Care (can also be claimed under Health 170688)
- Medical travel expenses within Canada (can also be claimed under 170688)
Health (170688) – Medical travel expenses within Canada or Out of Country Care for:
- Dental
- Drugs
- Health
- Vision
For an estimate (predetermination) of what your plan covers, go to Make a Claim > Need an Estimate? > Request an estimate > Start an estimate > Who is the estimate for? > Select a plan for this estimate.
Please ensure that your address is updated with your employer. Once your address is updated with your employer, it will be updated with Canada Life.
If you have access to Employee Self Service (ESS), you can update your address online:
Time and Pay > Employee Self Service > Personal Details
- Time and Pay: access from work (IDIR restricted)
- Time and Pay: access from home (IDIR restricted)
If you do not have access to ESS, call the BC Public Service Agency (1-877-277-0772) and a Service Representative will be able to update your information in PeopleSoft.
Pay Direct
Pharmacies, dentists, chiropractors, physiotherapists, naturopathic doctors, podiatrists, psychologists, massage therapists and optical stores/optometrists/ophthalmologists can register for Pay Direct through Canada Life.
If your service provider has signed up, simply provide them with your policy and ID number (and those for your spouse’s program, if you can coordinate benefits) and you will pay only the portion of the expense that's not covered under your benefits plan(s).
Extended health and drugs
To make a claim for reimbursement, you can submit a paper or electronic claim.
- Find the paper claim form on the Careers & MyHR forms and tools index page or My Canada Life at Work, and follow the submission instructions carefully. Make a photocopy of your expense receipt because the originals will not be returned to you
- Submit eClaims on My Canada Life at Work for prescription drugs, vision care, chiropractic, physiotherapy, podiatry, psychology, acupuncture, massage therapy and naturopathy
- Keep your original expense receipts in case you're asked to submit them
Once a claim is processed, you’ll receive a direct deposit if you’ve provided your banking information to Canada Life through My Canada Life at Work, otherwise, you'll receive a cheque in the mail.
All plan members are required to sign up for PharmaCare to assist with prescription drug coverage, limiting the impact on your lifetime maximum. In addition, some high-cost drugs will require you to apply for PharmaCare special authority before you can be reimbursed.
For information regarding drugs and medicines, please refer to the Extended health plan section.
Out of country emergency medical travel claims
Out of country claim forms are available on My Canada Life at Work and can be submitted online to Global Excel, by email to canadalife.claims@globalexcel.com or by mail following the instructions on the claim form.
Dental
Most dental offices will bill Canada Life directly when you provide your policy and ID number (and your spouse’s information, if you have coordinated benefits) and you'll pay only the portion of the service not covered by your benefits plan(s).
If your dentist cannot bill Canada Life directly (meaning, you have to pay the full cost at the dental office) or if you wish to claim to your Health Spending Account, you can submit a paper claim.
Find the paper claim form on the Careers & MyHR forms and tools index page or My Canada Life at Work and follow the submission instructions carefully. Make a photocopy of the expense receipt because the originals will not be returned to you.
Monthly orthodontic claims may be claimed through My Canada Life at Work.
Deadlines
It’s recommended that you submit claims immediately after treatment.
Late claims will not be accepted by Canada Life.
Extended health claims, including drug claims and dental claims, must be received no later than 15 months from the date the expense was incurred.
The claiming deadline for your Health Spending Account is February 28 following the year in which the expense was incurred.
For all claims questions, contact Canada Life at 1-855-644-0538.
Coordination of benefits
If your spouse is a BC Public Service employee and is covered under the BC Public Service benefits plan (excluding BC Ferries plan members), you're able to coordinate benefits and submit your extended health and dental receipts to both plans and get up to 100% of your eligible expenses reimbursed (subject to reasonable and customary limits and to plan limits).
If your spouse has Comprehensive coverage through the Flexible Benefits Program or another benefits plan, consider choosing the Coordination option to receive optimal coverage.
Insurance companies follow the guidelines below to determine which plan pays first, and how benefits are calculated.
- When you make a claim under coordinated plans, photocopy your receipt(s) and submit your claim to your plan first
- Once approved, you'll receive an Explanation of Benefits Statement. Now you can submit a claim to your spouse’s plan, along with the Explanation of Benefits Statement and photocopies of your receipt(s)
- Spouses will submit to their plan first, and to your plan second
- If you have dependent children, the order of submission is determined by your birthdays. If your birthday is earlier in the calendar year than that of your spouse, you'll submit your children’s claims to your program first
- Please note: if you have coordinated coverage and are submitting a predetermination to confirm reimbursement prior to purchase or service, the estimate will not reflect the coverage available under both plans. It will reflect coverage as if the item or service is being claimed under the primary plan only. Once the claim has been paid under the primary plan, you can submit your Explanation of Benefits Statement to a secondary plan to see if there’s further eligible reimbursement.
If you and your spouse have coordinated benefits and you're both covered under Canada Life, you can submit to both plans at the same time by filing an eClaim through My Canada Life at Work.
If not, you can submit a paper health claim form or dental claim form which you can find on the Forms and tools page or My Canada Life at Work.
If you have a Health Spending Account, use an Extended Health Claim with Healthcare Spending Account form or a Dental Plan with Healthcare Spending Account form to submit eligible expenses, both of which are also available on the Forms and tools page or My Canada Life at Work. The Health Spending Account is the last plan to claim from. Please note the deadline when submitting claims.
When coordinating benefits, please ensure the same names are being used on both plans (for example: legal names) so there are no delays with the coordination of benefits with the carrier. If the names do not match, there may be a delay in payment, or payment may be missed.
Once your claim is processed, you'll receive notification. If you provided Canada Life with your banking information, they’ll deposit the reimbursement into your banking account. Otherwise, you'll receive a cheque in the mail.
A retiree plan will always pay after any group plan that covers you as an employee.
If coverage under the secondary plan is terminated, please contact Canada Life at 1-855-644-0538 or via email through My Canada Life at Work to ensure that claims are paid correctly.
