4.1 Claims by Offline and Out-of-Province Providers
[November 11 2025: Updated for clarifications]
General Policy Description
Some PharmaCare providers are not connected to PharmaNet. They or their clients must submit claims to PharmaCare manually. These PharmaCare providers are:
- Offline providers: Non-pharmacy providers in B.C. who opt out of connecting to PharmaNet
- Out-of-province (OOP) providers: Providers outside of B.C. who cannot connect to PharmaNet; connection to PharmaNet must be within B.C.
This section provides information for providers who are not connected to PharmaNet, but who participate in PharmaCare.
Policy Details
Non-pharmacy providers in B.C. may opt out of connecting to PharmaNet. These are offline providers.
Some out-of-province (OOP) providers can enrol in the PharmaCare program in order to submit claims to PharmaCare or enable their patients to be reimbursed by PharmaCare but they cannot access PharmaNet since access to PharmaNet is restricted to sites in B.C.
Offline and OOP providers may submit manual claims to PharmaCare (i.e., by mail, fax or courier) for benefits provided to B.C. residents through PharmaCare’s 100% coverage plans (Plans C, D, F, G, W and Z).
Offline and OOP providers should not submit manual claims to PharmaCare for benefits provided to B.C. residents under Fair PharmaCare (Plan I). These beneficiaries may submit claims using the Manual Patient Claims process detailed in Section 4.2—Manual Patient Claims (providers should support their claims by providing them with a receipt showing the amount was paid in full).
OOP sites enrolling as providers are required to sign a declaration. By signing the declaration, OOP providers agree to serve the residents of B.C., to be bound by the laws of the Province of B.C. and to have any court proceedings related to their enrolment in PharmaCare conducted in B.C.
If enrolment is approved, the site becomes a PharmaCare provider, but is not connected to PharmaNet.
OOP providers are subject to the same policies and procedures as in-province providers.
Payment is not made for B.C. residents visiting an OOP community; payment is provided only because the OOP provider is closer or more accessible to a B.C. resident’s home than the nearest B.C. provider. However, in some limited circumstances, payment is also made because an OOP provider has been approved to sell certain products to B.C. residents that will be covered by the PharmaCare program.
Offline and OOP providers should note that an individual ceases to qualify for PharmaCare coverage on the day they leave B.C. to reside elsewhere, even though Medical Services Plan (MSP) coverage may continue.
Offline and OOP providers may opt out of PharmaCare at any time, but if they do so, their clients will not be reimbursed by PharmaCare for purchases made at their site.
All claims by providers are subject to PharmaCare Audit.
Procedures
Manual claims
PharmaCare adjudicates manual claims using the PharmaNet system.
Several claims can be submitted manually at the same time under one invoice. If a manual claim is accepted, payment for the PharmaCare portion is issued by the Ministry of Finance, and a statement (the "remittance advice") is sent by PharmaCare to the provider. The remittance advice itemizes the processed claims.
Documentation submitted with a claim that is accepted is not returned.
Claims that are accepted and processed are returned to the provider with a remittance advice. Claims that are not processed because they are incomplete or incorrect, are returned to the provider without a remittance advice. For more information, refer to Incomplete/Incorrect Claims below.
Direct deposit payments
The Ministry of Finance issues payments to providers for accepted claims. To receive payment by electronic funds transfer, complete a British Columbia Government Direct Deposit Application. Submit the application and an original void cheque to:
PharmaCare Information Support
PO Box 9655 Stn Prov Govt
Victoria BC V8W 9P2
The Direct Deposit Application is in the PharmaCare Welcome Package sent to new providers, and additional copies are available from Health Insurance BC (HIBC) Info Support at informationsupport@hibc.gov.bc.ca.
All manual provider claims must include:
- A completed PharmaCare Claim Form (HLTH 5336)
- A record of the details of each individual product dispensed
- A work order/invoice, with costs itemized
- A completed PharmaCare Prescription Invoice (HLTH 5335), which summarizes the total number of claims and total dollar value of the invoice submitted
Up to 100 claim forms may be submitted with one Prescription Invoice.
Ensure that all the following information is provided and that the correct units of measure are used. If unsure of the unit of measure to use for a particular product, consult the Correct Quantities list.
- Complete a PharmaCare Claim Form for each product or service (even if multiple products/services are provided for the same patient), recording:
- Patient's name and Personal Health Number (PHN)
- Date (YYY/MM/DD) that the device or service was provided
- Name of the provider to whom payment should be sent
- Provider's Site ID
- PharmaCare plan (C, D, F, G, W, or Z)
- Prescribing physician 's MSP billing number, or prescribing nurses’ college ID
- Provider's work order or invoice number
- Full quantity of the drug or product covered by the claim. See Correct Quantities
- CDIC No. – the DIN (for drugs) or the PIN (for compounds or products). Refer to the lists of PINs at Information for Pharmacies and Information for Device Providers
- Dispensing fee (up to the PharmaCare maximum)
- Ingredient cost (up to maximum covered by PharmaCare). See Sections 5.6—5.22
- Total claimed – total $ of Dispensing Fee and Ingredient Cost
- Balance due – same as total claimed
- Patient/agent's signature (an agent may be the parent of a child patient or someone with Power of Attorney for a patient)
2. Submit the top copy of each PharmaCare Claim Form to PharmaCare with supporting documents such as work orders or invoices (up to 100 Claim Forms can be sent in with each Prescription Invoice). Give the second copy to the patient. Retain the third copy for your records. 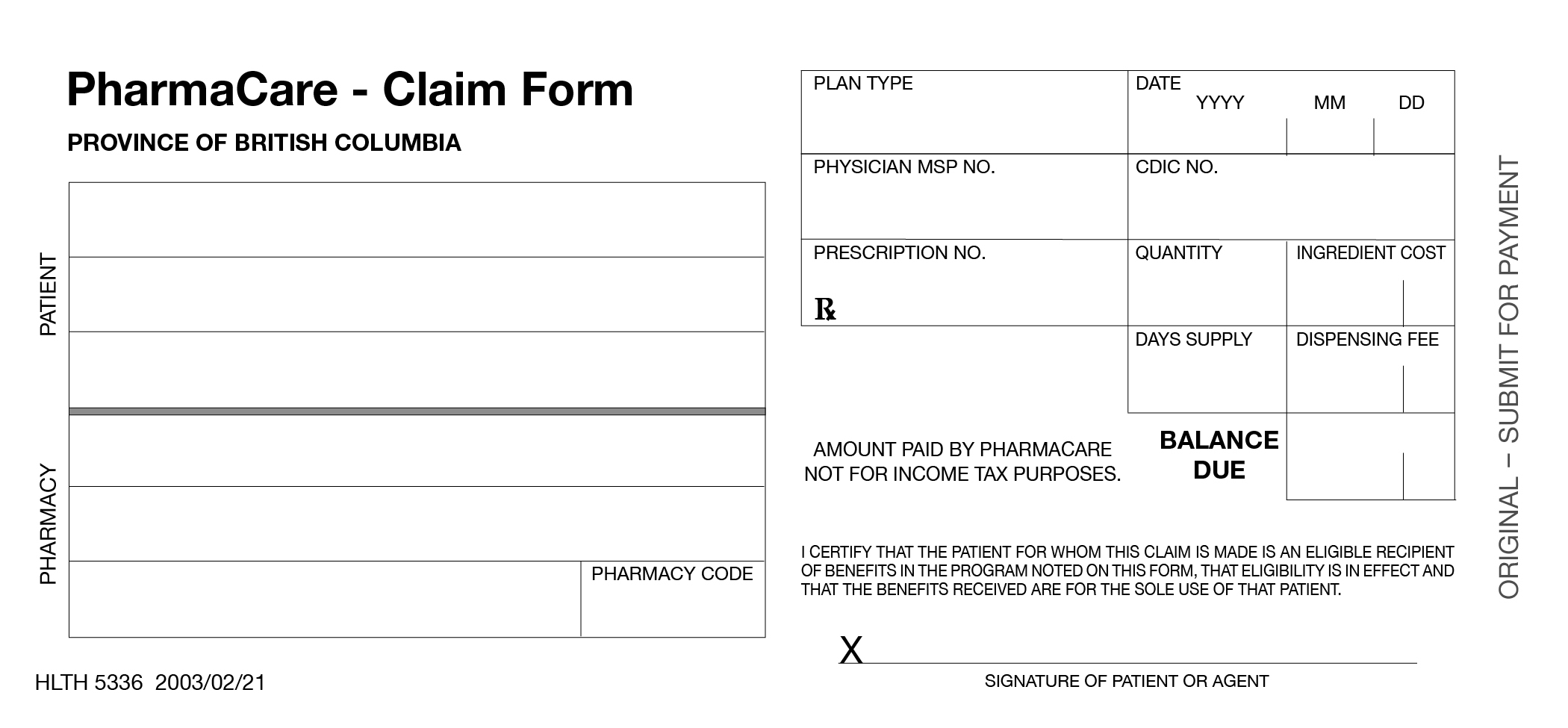
PharmaCare Prescription Invoice (HLTH 5335)
Complete the invoice, with the following information:
- Pharmacy ID - provider's name and address
- Date of the invoice (YYYY/MM/DD)
- Total number of claims being submitted with the invoice
- Provider's Site ID
- Total amount invoiced - total $ amount for all the claims covered by this invoice
- Signature - Provider's authorized representative's signature
- Position or title of the person who has signed the invoice
Submit the Prescription Invoice with up to 100 claim forms and associated documents by mail to:
PharmaCare
PO Box 9655 Stn Prov Govt
Victoria BC V8W 9P2
Retain the second copy of the invoice (labelled PHARMACY) for your records.
Forms may be couriered to:
2261 Keating Cross Road; Block B - Unit #200
Saanichton, BC V8M 2A5
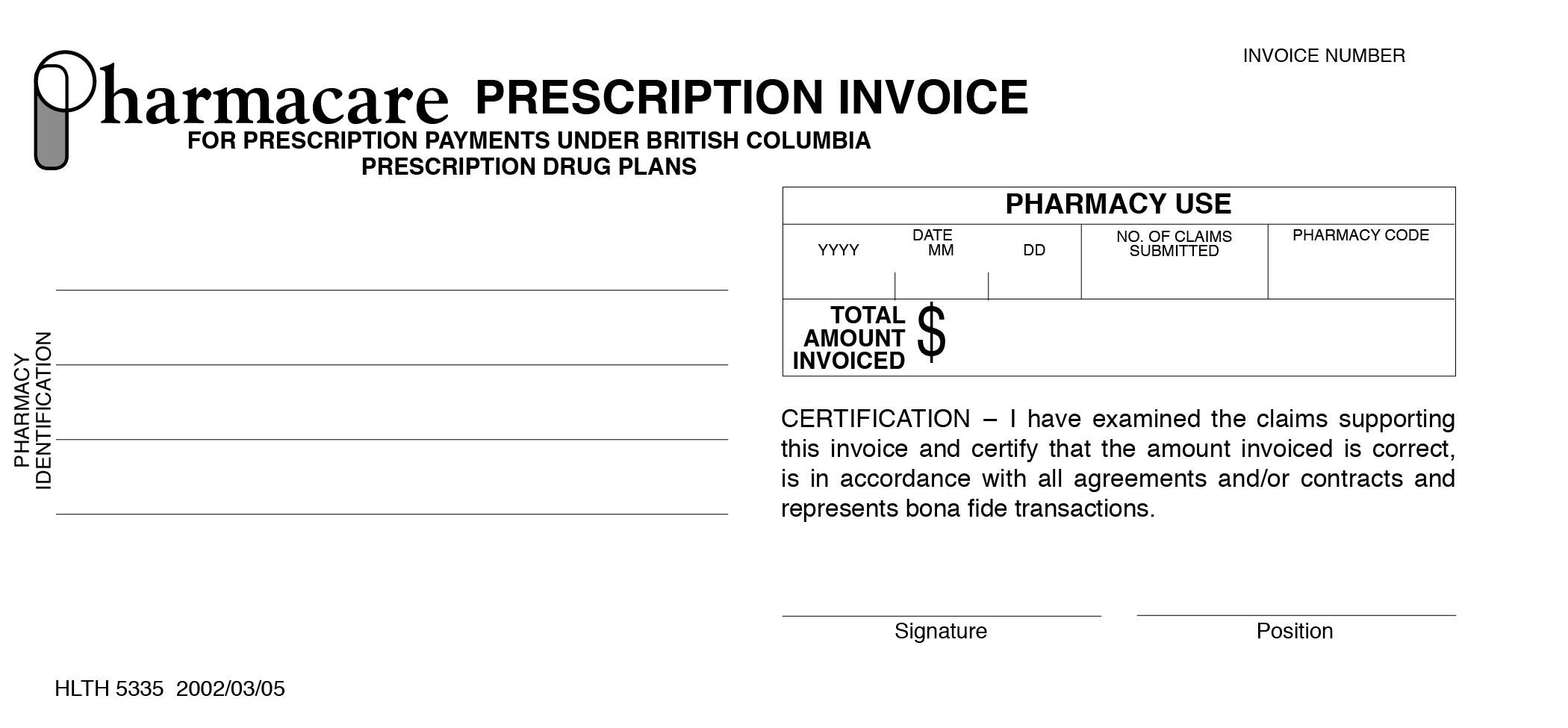
Processed claims are returned with the remittance advice. PharmaCare returns claims that cannot be processed to the provider for correction or completion. PharmaCare deducts the amount of the incomplete or incorrect claim(s) from the invoice total. The Prescription Invoice is not returned.
If an incomplete or incorrect claim is returned to you:
- Correct or complete the original form; do not submit a new claim form.
- Ensure the date on the claim form is the date the client received the product or service.
- Include the $ amount of the corrected claim on a new PharmaCare Prescription Invoice.
- Submit the Claim Form and Prescription Invoice to HIBC.
If the claim is rejected due to patient ineligibility or because the product is not a benefit, the claim form is returned. These claims should not be re-submitted.
