Managing Patients with Pain in Primary Care - Part 1
Effective Date: Feb 23, 2022
Recommendations and Topics
- Preamble
- Scope
- Key Recommendations
- Definition
- Epidemiology
- Approach to Care
- Assessing and Managing Pain
- Acute Pain
- Subacute (4 weeks - 3 months) - Transition from Acute to Chronic Pain
- Chronic Pain (3+ months)
- Procedural Pain Management (PPM) for Patients in Primary Care Settings
- Substance Use Reduction
- Considerations for Referral or Request for Expert Input
- Managing Pain in the Older Adult
- References
- Practitioners Resources
- Resources for Patients
- Appendices
Preamble
Managing patients with pain, especially chronic non-cancer pain (CNCP) is challenging given current practice realities. Practice patterns have changed with more patients receiving episodic care from walk-in-clinics, emergency departments, and group or team-based clinics with a variety of participating clinicians. Clinicians can be overwhelmed by guidelines, updates, algorithms, portals, and on-line journals. The British Columbia’s Opioid Overdose Crisis has permeated our day-to-day practice and often create prescribing uncertainty. Many have fears (though often misplaced) about potential disciplinary and legal consequences from licensing and legislative bodies. Patients also have access to many sources of information, may come with a history of past trauma and unequal treatment by the health care system, and often struggle with reduced function and ability because of their pain.
The intent of this guideline is to provide practical, accessible, and BC specific guidance. In essence, this is more of a Clinical Guidance Document and not a formal guideline. It’s a distillation of many guidelines, expert recommendations, and standards of care. There are few overall pain guidelines for direct comparison. The guideline development working group were made aware of the Appraisal of Guidelines for Research and Evaluation (AGREE) process that helped inform their appraisal of these guidelines.
There is no clear or absolute clinical pathway to managing pain and many controversies persist, especially in the use of opioids and cannabis. The guideline development committee recommends reasonable clinical judgement, clear documentation, and frequent reassessment.
Scope
This guideline comprises of two parts:
- Pain Assessment and Management Approaches
- Pain Management - Pharmacological and Procedural
Within scope of this guideline:
- Practical recommendations within the primary care setting for a graded, multimodal approach to supporting adult patients (≥ 19 years) with pain on a continuum from acute, subacute to chronic pain. A multimodal approach is one where patients with pain receive multiple interventions and supports, both concurrently and sequentially.
- General approaches to treating patients with pain and links to supportive resources.
Out of scope of this guideline:
- Detailed recommendations for condition-specific pain.
- Pain in palliative care or as part of an advanced life-limiting disease.
- Refer to BC Guidelines: Palliative Care Part 2: Pain and Symptom Management. Patients with pain associated with serious or advanced illness may benefit from both the Palliative Care and Managing Pain guidelines.
- Pain in children or young adults. Consider accessing the Pain Service at BC Children’s Hospital for more specific assistance in managing pain in this age group.
Key Recommendations
- Patients with moderate to severe acute injury should receive adequate pain control and consideration of early referral to specialized services, where indicated and available.
- Consider improving function and reducing disability, rather than elimination of pain, as the goal of pain management strategies, especially when pain progresses into the chronic pain continuum.
- A supportive longitudinal therapeutic relationship is a foundation of pain management. Given the changing face of primary care with team-based care, walk-in care, and virtual care, use of databases like Electronic Medical Records (EMRs), PharmaNet, and CareConnect is increasingly important.
- Throughout the pain continuum, especially in subacute and chronic phases, assess for biopsychosocial factors (yellow flags) and co-morbid conditions. Be alert to addressing risk factors for developing chronic pain.
- Complex Regional Pain Syndrome (CRPS) is often considered a pain emergency and warrants urgent referral or consultation by a pain specialist and consideration of early intervention with steroids.
- Consider all forms of interventions, including non-pharmacological and pharmacological, as a ‘trial’ to be reassessed for effectiveness on a regular basis.
- For people with chronic pain not already on opioid therapy, optimize non-pharmacotherapy and non-opioid pharmacotherapy first before considering a trial of opioid therapy.
- For all medication, aim for the optimal dose and be aware of the recommended maximal dose with fewest side effects and do regular, recurrent evaluation to assess for meaningful improvement in pain and function. See Managing Pain in Primary Care - Part 2: Pharmacological Management.
Definition
The International Association for the Study of Pain (IASP) defines pain as “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
In addition, six key notes are added.
- Pain is always a personal experience that is influenced to varying degrees by biological, psychological, and social factors.
- Pain and nociception are different phenomena. Pain cannot be inferred solely from activity in sensory neurons.
- Through their life experiences, individuals learn the concept of pain.
- A person’s report of an experience as pain should be respected.
- Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being.
- Verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain.
While it is convenient to try and categorize pain in terms of mechanism, duration or origin, there can be significant differences in how individuals experience pain and how tissues may heal. The parameters for defining pain as acute or chronic may vary depending on the type of trauma and past history, which suggests that a more nuanced approach to applying a framework for resolution of the pain is often required.
Acute pain is pain generally expected to last less than 4 weeks and occurs within the context of tissue damage and repair, resolving with tissue healing.
Subacute pain (transition zone between acute and chronic) is defined as pain not resolving or diminishing as expected in 4-12 weeks after initial onset. The ‘subacute’ timeframe should trigger practitioners to pause and reflect on progress of pain management and take steps to reduce the likelihood of transition to chronic pain.
Chronic or persistent pain is pain persisting for greater than 3 months. It can arise from long-term medical conditions not expected to improve such as osteoarthritis, scoliosis, and multiple sclerosis, or it can also be pain that persists beyond expected time of healing.
Pain can be described in terms of mechanisms. Treatment modalities, including adjuvants, may differ significantly depending on the mechanism of pain.
- Nociceptive: arises from actual or threatened damage to underlying tissue (e.g., soft tissue, bone, viscera)
- Inflammatory: perception of noxious stimuli that occur during an inflammatory or immune response.
- Neuropathic: results from damaged or dysfunctional nerves (leads to misfiring pain signals).
- Nociplastic: altered pain perception without clear evidence of actual or threatened tissue damage such as in fibromyalgia.
When considering a patient’s experience of pain, it can help to remember:
- Pain is always a personal, learned experience that is influenced to varying degrees by biological, psychological, social, and cultural factors and life experiences.
- A person’s report of their subjective experience of pain should be respected.
- Although pain usually serves an adaptive role, it may have adverse effects on function, and on social and psychological well-being.
- Verbal description is only one of several ways to express pain; inability to communicate does not negate the possibility that a person experiences pain.
Epidemiology of Chronic Pain
According to Statistics Canada, an estimated 7.6 million, or one in five people (across their lifespan) in Canada, live with chronic pain.1 It is estimated that 1 in 5 adults in BC suffer with chronic pain.2
Approach to Care
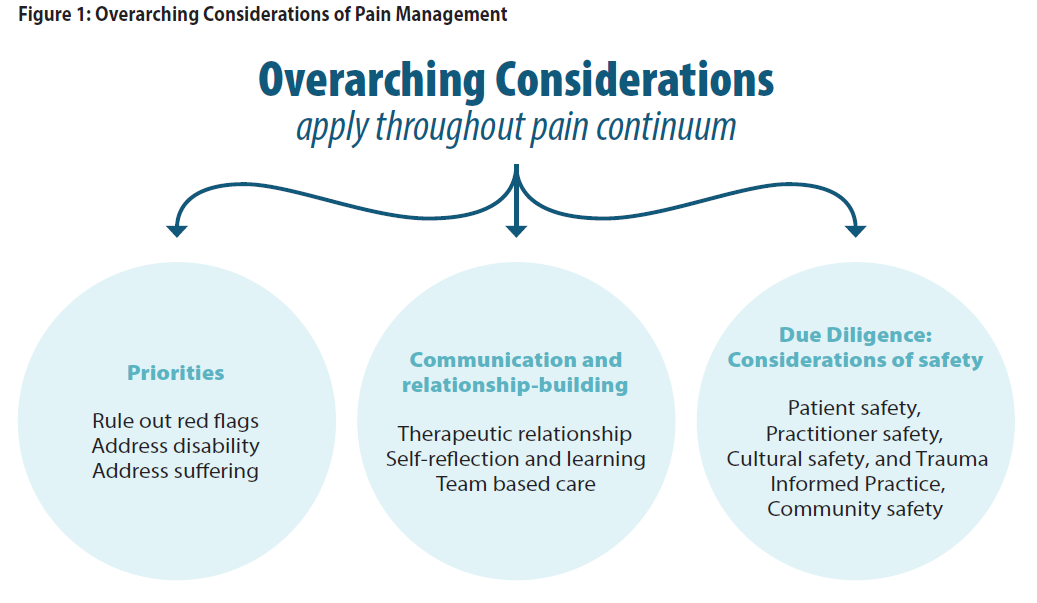
Pain management is within the scope of practice of all primary care practitioners. Patients seeking management of their pain may at times face social stigma and negative assumptions about their motives, leading to less than adequate care. Successful pain management requires a highly individualized, respectful, evidence-informed treatment approach and benefits from a team-based, biopsychosocial approach. See Appendix A: Overarching Considerations of Pain Management.
General Principles
Many groups, especially Indigenous, people of colour and immigrant communities, may be disproportionately affected by their past experience of inequitable treatment by healthcare providers. However, many of these communities may also bring strength, resilience, protective factors (cultural continuity), and other strategies for self-management, such as traditional medicine and healers.
While clinicians may see a patient at any point along the pain continuum, the principles for managing pain remain consistent. It is important to develop a positive, supportive, and respectful therapeutic relationship. Strong consideration should be given to using a trauma informed approach, especially in people experiencing chronic pain.
- Emphasis on addressing ongoing impact of pain, disability, and suffering. The goal is improved function – use functional assessments for personal and occupational functioning.
- Unattached patients and those in team-based practices with a variety of care providers present a challenge to the traditional long-term relationship that clinicians have previously had. Use of the EMR and shared databases such as PharmaNet and CareConnect are increasingly important to connect the information relating to patient’s history and past care interventions.
- Encourage supported self-management strategies (See Resources: Resources for Patients) and incorporate into daily lives.
- Consider all interventions and therapies as therapeutic trials.
- Consistent re-evaluation of progress is important. Address early if progress is delayed.
- Red flags suggest a more urgent need for investigations or referral (Table 1: Pain Red Flags).
- Yellow flags are physical, psychological and social Factors that may affect development of chronic pain (Table 2: Pain Yellow Flags)
- Be alert to red and yellow flags - assess and re-assess concurrent disorders and biopsychosocial factors that increase the risk of the pain becoming chronic. Be mindful of patient, practitioner, and community safety.
- Document well - improvements/changes in symptoms and function, and patient assessment of effects of individual modalities. This is especially important when using opioids and if exceeding recommended prescribing standards.
Assessing and Managing Pain
Overview of Strategies for Managing People with Pain
This figure describes management strategies over time from initial onset, highlighting a stepped approach to patients with pain, the need to assess progress and consider additional or alternate strategies, including mitigating risk of progression.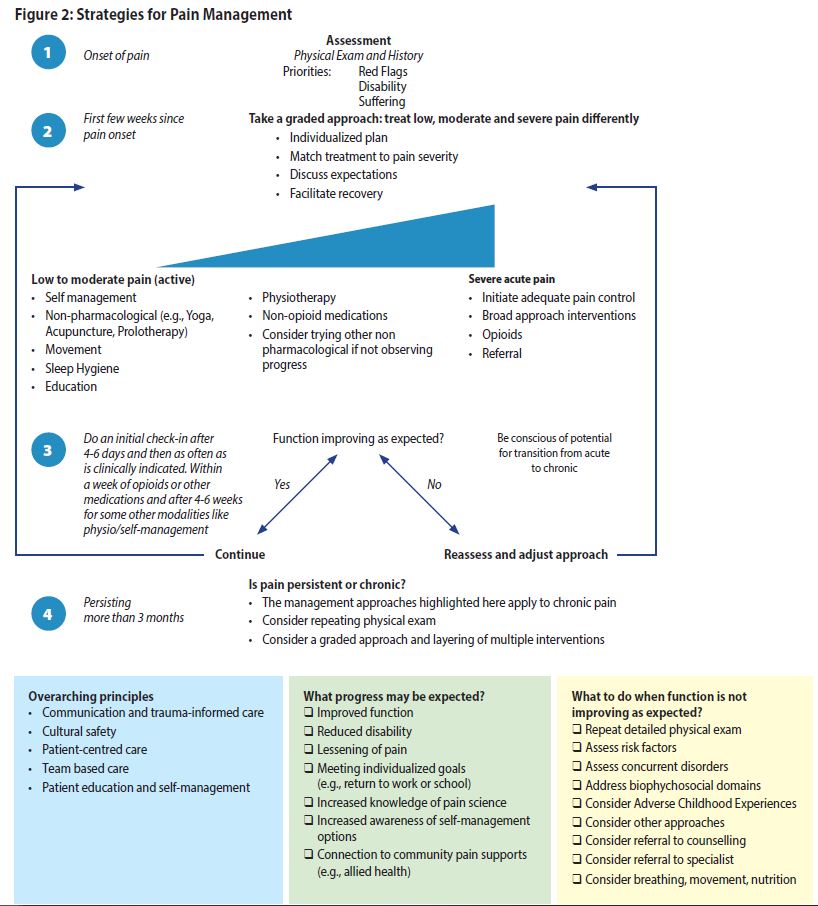
Acute Pain
Assessment
- Identify the source of the pain. Consider pain mechanism and location.
- Take a structured pain history. Consider one of the following strategies:
- OPQRST – Onset, Provoking/Palliating, Quality of pain, Region/Radiation, Severity, Timing/Treatment.
- AAA - Alleviating/aggravating factors, Associated symptoms, Attributions/adaptation.
- Consider assessment for mood disorder and substance use disorder.
- Assess early for Red Flags. See Table 1: Pain Red Flags below.
Table 1: Pain Red Flags 3 Red Flags suggest a more urgent need for investigations and/or referral (adapted from Centre for Effective Practice 'Management of Non-Cancer Pain').
| Red Flag Category | Clinical Features |
|---|---|
| Neurological | Diffuse motor/sensory loss; progressive neurological deficits; Cauda Equina Syndrome |
| Infection | Fever, chills, weight loss, IV drug use, immunocompromised (including steroids) |
| Fracture | History of physical trauma; minor trauma in elderly or with osteoporosis risk (consider acute vertebral fractures) |
| Malignancy | History of cancer; age >50; unexplained weight loss; night pain or supine pain; severe fatigue |
| Inflammatory | Acute monoarthritis; Arteritis-giant cell/temporal; acute vasculitis; acute flare up of connective tissue disease |
| Vascular | History of significant vascular risk factors, clotting disorders, and cardiovascular disease; hemodynamic instability; abdominal pain suggestive of AAA; unilateral limb symptoms including swelling and absence of pulses, coldness |
| Constitutional | Unexplained fever (>38°C); unexplained weight loss; night sweats |
| Complex Regional Pain Syndrome (CRPS) | Previously known as Reflex Sympathetic Dystrophy, an evolving CRPS is usually considered an emergency by pain specialists with a strong suggestion for at least a phone consultation and consideration of an urgent referral. While considered rare, it is occasionally progressive involving the arm, leg, hand, or foot. Symptoms may include excessive pain, swelling, and changes in skin colour, texture, and temperature. A subset of patients may benefit from early steroid therapy so again consider an urgent consultation and referral. |
Functional and Occupational Assessment
Support work rehabilitation, occupational review and return to work or education. Explore work accommodation options (e.g., part-time, modified duties), if appropriate, rather than complete disability.
- For WorkSafeBC and Insurance Corporation of British Columbia (ICBC) injuries, consider early intervention support and consultation.
- Many occupational groups, employers and insurance companies have occupational health departments and clinician experts. Engage early if complex pain or extended disability is anticipated.
Management
- Patients with painful acute injury or illness should receive appropriate pain control. See Managing Pain in Primary Care – Part 2: Pharmacological Management.
- To help reduce the pain burden, consider focusing on medication in the first few weeks. This may allow the patient the time and confidence to begin to engage in other pain treatment modalities that are not medication based. See Appendix B: Non-pharmacological Treatment Modalities for Pain.
- Consider non-opioid medications first unless pain is severe.
- If considering prescribing opioids, assess for active and past substance use disorder (SUD) (including nicotine, alcohol, opioids, marijuana) and psychiatric disorders. The presence of these disorders is not a reason to not prescribe but suggests a need to proceed with caution and to have a clear discussion with patient about risks. The presence of any SUD is not an absolute contraindication to prescribe opioids, though it does increase risk of overdose and addiction to opioids. Thus, more safeguards, including enhanced monitoring, need to be put in place and clear documentation of risks and benefits for that particular patient outlined. Certain pain medications may not be safe to prescribe. Patients with pain when on opioid agonist therapy (OAT) need to be referred to an addiction medicine specialist with knowledge of pain treatment. Specific management for individuals in this situation is outside the bounds of this guideline.
- If opioids are prescribed for acute pain, suggest limiting the duration of the first prescription of opioids to less than 7 days, and use short-acting agents only.4
- If patient is not progressing, try alternate interventions and assess if pain is becoming more complex (refer to Subacute section below).
- It is always appropriate to consider non-pharmacologic strategies such as chiropractic care, manual therapy, and acupuncture (as examples) in the acute onset of pain.
Subacute (4 weeks - 3 months) - Transition from Acute to Chronic Pain
Assessment
If the patient is not progressing as expected after 4-6 weeks (e.g. severe pain, pain is increasingly complex, multiple pain sites), assess for biopsychosocial factors (Yellow Flags) that may indicate risk for developing persistent pain and disability (See Table 2: Yellow Flags). Consider asking “How is the pain affecting the rest of your life?”
Table 2: Yellow Flags - Physical, Psychological and Social Factors that May Affect Development of Chronic Pain (adapted from Centre for Effective Practice)3,5,6
| Physical Factors | Psychological Factors | Social Context |
|---|---|---|
|
Lack of activity/prior deconditioning Increasing age (levels out at age 60) Early and high levels of disability Duration or intensity of pain, disproportional to mechanism of injury Multiple somatic complaints such as fatigue, insomnia, anorexia Previous injury and/or comorbid conditions, particularly if prolonged recovery |
Depression6 Anxiety Post-Traumatic Stress Disorder (PTSD) Adverse Childhood Experiences History of sexual abuse9 Anger, fear, hypervigilance Past/present history of substance use |
Injured at work; low job satisfaction; challenging work relationships; awareness of work safety issues On-going litigation or compensation issues Poor support structure (family and social) Family history of chronic pain Motor Vehicle Accident Vulnerable populations (e.g., social determinants of health such as poverty, lack of stable housing, physical or mental/ cognitive challenges, language and cultural barriers, frail elderly) |
Management
Take steps to mitigate development of chronic pain. This may be the time for more careful reflection. Pain persisting more than a few weeks and/or beyond what may be considered normal healing and repair is a cue to consider the whole patient and address biopsychosocial factors and socioeconomic factors in parallel with other interventions.
Reflection should include:
- Are there specific patient-related issues such as past traumas, previous addictive behaviours, financial/social/housing insecurity, or other medical conditions?
- Are there practitioner-related issues including personal experiences with pain, personality differences, and time constraints.
- Is pain getting more complex? What else can be done?
- Consider repeating a detailed and/or targeted physical exam.
- Initiate or repeat assessment tools to monitor progress such as:
- Practice Support Program (PSP) and Pain BC have a more extensive list of pain assessment tools.
- When using the assessment tools, some pain specialists have noted that many patients will label every domain as 10/10. While it may not be an accurate reflection of the actual pain, it may reflect the patient’s overall frustration and hopelessness and should not be dismissed as malingering or over-exaggeration. Consider that multiple pain mechanisms may now be involved in the patient’s experience of pain.
- Re-emphasize that total elimination of pain may not be the goal. Improving function and managing suffering are the priorities. Provide information on pain education and self-management. See Resources: Resources for Patients.
- If recovery is delayed, refer to specialists for expedited assessment or for specialized treatments/ procedures (e.g., epidural or nerve root injections, facet or SI joint injections, joint injections or vertebroplasty). For some conditions such as CRPS and worsening neuropathic pain, referral to specialty services should be as early as possible. This may be especially true in frail older adults as they experience greater functional impairment that can worsen frailty.
- As complexity increases, consider combinations of treatments rather than a sequence of treatments. Consider other options, in addition to medications and non-pharmacological interventions. Consider involvement of allied health professionals and/or teams, where available. See Appendix C: Allied Health Professionals to Support Pain Management.
- Explore accommodations for work/school such as the WorkSafeBC Physician's Report.
- For patients involved in motor vehicle accidents who are not recovering as expected or have an unknown diagnosis or complicating factors, consider referral to an ICBC registered care advisor (RCA) within 90 days of the accident for an expedited medical consultation.
Chronic Pain (3+ months)
Assessment
It may be worthwhile considering a slightly different approach if the patient has long standing and well documented pain, versus the patient who has recently developed chronic pain after an acute event. Many strategies are the same, but a patient with long standing chronic pain may have adapted to achieve some stable level of function and ability, while a patient with new onset of chronic pain may still be uncertain about work options and activities of daily living (ADL) adaptations.
Evaluating and managing patients with chronic pain requires repeat history and physical exams as well as evaluation of disability and psychosocial domains. This can be beneficial even for long-term patients who appear stable. This process can be conducted over multiple office visits and may at various times include:
- Repeat / review history, physical exam
- Consider asking yourself:
1. What is going on?
2. Could it be something else?
3. Could two things be going on at once?
4. Is the diagnosis still supported by the available evidence? - Review medication history including over the counter (OTC) and “off label” products (including use of cannabis)
- Repeat / review pain assessment tools, including functional and occupational assessments
- Assess / reassess for mental health conditions (e.g., use screening tools for anxiety, depression, PTSD).
Both chronic pain and depression may frequently co-exist, especially in old age, and may be risk factors for each other.10 Consider exploring other life changes as possible contributors to depression and/or pain symptoms. What other things are going on in your life?”
- Assess / reassess concurrent disorders and other medical conditions:
- Substance use disorders (e.g., opioid, alcohol)
- Sleep disorders
- Chronic diseases (diabetes, chronic heart failure, obesity, cancer, osteoporosis)
- Falls and falls risks, especially in frail older adult (refer to BCGuidelines: Falls Prevention)
- Polypharmacy, including OTC medications
- Cognitive and/or sensory impairment
- Assess / reassess risk factors and biopsychosocial domains (Red and Yellow Flags)
- Consider referral to specialists or allied healthcare. Appendix C: Allied Health Professionals to Support Pain Management.
- Consider strategies such as breathing, movement, and nutrition. All strategies may add to the layering effect that improves function and reduces suffering and disability. See Appendix B: Non-pharmacological Treatment Modalities for Pain.
Management
- In B.C., many of these modalities are not publicly funded and availability of specialized care may not be equitably available. Access to many specialized pain management services outside of a few large urban centres is often extremely limited. Some of this can be mitigated through “telehealth” type options, which more specialists are using.
- However, many patients who qualify for income or disability assistance may receive coverage or partial coverage for non-insured health benefits (NIHB) such as physical therapy, acupuncture, chiropractic care, massage therapy, mental health care, pharmacy coverage, medical supplies, and dental care. For more information see BC Family and social supports.
- Federal employees, RCMP members, armed forces personnel, and military veterans may also have additional health benefits coverage.
- Best practice treatment plans involve primary care providers working closely with allied health care providers, such as physiotherapists, occupational therapists, psychologists, chiropractors, massage therapists, and social workers, and should be centred around patient education and self-management. Despite many services not being publicly funded, explore coverage through ICBC, WorkSafe BC and patient’s work disability services or private insurance, in addition to coverage through income assistance. Refer to Pain BC and PathwaysBC for listings of providers, self-management groups and clinics with experience and training in managing chronic pain.
- Match non-pharmacological interventions that are best suited to patient’s specific pain mechanism and history, such as physiotherapy or chiropractic therapy for mechanical low back pain (LBP); psychological intervention if there is a possible history of PTSD or Adverse Childhood Experiences (ACEs); Cognitive Behavioural Therapy (CBT) for depression and anxiety; and social work or occupational therapy if housing/financial/job insecurity are present. Using a layered and multimodal approach may be more effective than trying a single intervention at a time. For information on services available in the community, visit Pain BC and HealthLinkBC.
- Discuss goals of care. Specifically, improved function, reduced suffering, and patient’s other individual goals, and not necessarily removal of all pain.
- Review patient expectations for treatment outcomes and address misconceptions or unrealistic expectations.
- Over multiple visits, develop an Individualized Care Plan or chronic pain flow sheet3 to encourage a better systematic approach to chronic pain. Share and review the plan with the patient.
- Provide guidance for practical steps that can be addressed in next visit.
- If a patient has been adherent to therapy for 3-4 months and is not responding, consider an alternative approach.
- Educate patients about chronic pain and the multidimensionality of pain. See Resources : Resources for Patients. It is often assumed that tissue damage will continue to heal, but there may be other interfering factors.
- Educate patients that non-opioid treatment gives equal pain control and fewer side effects than opioid treatment for most types of chronic LBP and knee and hip arthritic pain.11
- Educate patients that opioid use may increase pain sensitivity and add to pain at injury sites during withdrawal.12, 13
Procedural Pain Management (PPM) for Patients in Primary Care Settings
Within the context of primary care, there are several procedures that can be within the scope of most clinicians. The College of Physicians and Surgeons of B.C. (CPSBC), in accordance with the BC Medical Quality Initiative (BCMQI), categorizes procedures into four tiers (basic, intermediate, advanced I and advanced II). Basic and intermediate procedures include:
- Trigger point injections
- Bursa injections
- Intra-articular injections including the hip and intra-articular glenohumeral joints
- Mid-sized peripheral nerve blocks
These procedures generally don’t require imaging, can be performed in an office setting and are not restricted to an accredited facility. It is beyond the scope of this guideline to describe these procedures in detail and their indications, but they tend to be self-explanatory, and several online instruction resources exist.
For more complex procedures (e.g. epidural injections, facet joint injections, sympathetic nerve blocks) the BCMQI has described these procedures as Advanced Level I and II, which are required to be done in an approved facility or hospital. Delivery of these procedures in non-hospital settings (e.g., community based GP practices) require facility accreditation and practitioner credentialing. Refer to CPSBC and BCMQI websites for more information.
Substance Use Reduction
A number of different psychoactive substances have been shown to temporarily supress pain perception in the euphoric phase (the reason the patient with pain may like the feel of the substance). Yet, these same substances can increase pain sensitivity and add to chronic pain in the long run. Alcohol, tobacco, and opioids are all examples.13–16 Patient education on this topic then a trial of tapering down or off of these substances may be needed to help pain perception. In those with CNCP, opioids can produce a dose-dependent pain sensitization that temporarily worsens during tapering.12, 17, 18 For those with chronic pain or an opioid use disorder, previous injury sites can hurt again during abrupt withdrawal and add to the risk of opioid re-initiation. Thus, slow tapering along with the use of adjuvant medications like non steroidal anti-inflammatory drugs (NSAIDS) or gabapentinoids may be helpful in adults who do not meet an OUD diagnosis. Previously stable OAT or opioids used for the treatment of OUD should not be routinely tapered.
Supported Self-Management
- Provide or refer patient to educational resources about science of pain. Pain education has been shown to decrease disability and increase self-efficacy.19 Refer to Resources: Resources for Patients for helpful resources.
- Provide patient with information about self-management (including focused breathing, nutrition, gentle movement, mindfulness meditation, sleep hygiene, etc.) connecting to additional support (e.g., community physical activity programs, dietitians, etc.).
- Consider goal setting, including return to work and Brief Action Planning (BAP).
Allied Health Professionals to Support Non-pharmacological Pain Management
Pain BC has developed an overview of Allied Health Approaches To Chronic Pain Management-A Tool For Primary Care Providers. Many non-pharmacological interventions may be partially or fully covered by third party insurers (e.g., ICBC or WorkSafeBC), or if patient is on disability or income assistance. See Appendix C: Allied Health Professionals to Support Pain Management for more details on allied practitioners.
Considerations for Referral or Request for Expert Input
When patients DO NOT experience ongoing improvement in function and decrease in suffering then consider:
- Consultation with an appropriate specialist.
- Structural cause such as a compression fracture.
- Psychological services if history of PTSD, ACEs, or catastrophizing.
- Pain clinic if pain appears to have a nociplastic component.
Guiding principles for referral or request for expert input:
- Not seeing appropriate progress and pain looks likely to persist longer than expected.
- Neuropathic features develop, persist, or worsen.
- Post-op patients unable to reduce or discontinue opioid use.
- If patient is continuing to show biopsychosocial factors that increase risk of progression to chronic pain.
- Some pain specialists suggest that the emergence of CRPS symptoms warrants at least a phone consultation to assess the need for urgent referral. If WorkSafeBC or ICBC involved, phone the worker’s medical advisor and ask for an expedited appointment.
- If an interventional or surgical procedure is likely.
- If chronic non-cancer pain and OUD coexist a referral to an addiction specialist is warranted.
Managing Pain in the Older Adult
Managing pain in the “Older Adult”, especially the frail older adult, often requires modifications and adjustments in both approach and dosages. Many experts suggest that age greater than 70 may be an appropriate age to consider age related factors in assessing and managing pain. The definition of frailty is still being fully defined but its current definition is a medical syndrome with multiple causes and contributors, characterized by diminished strength and endurance and reduced physiological function, leading to increased vulnerability for adverse health outcomes such as functional decline and early mortality. While frailty is common with increasing age, it is not an inevitable part of aging. Additional information about Healthy Aging and Preventing Frailty can be found in the updated provincial healthy aging strategy.
Guiding Principles:
- The frail older adult may require adjustments in medications and dosages, but the use of opioids is not contraindicated. See Part 2: Pharmacological Treatment for more specific guidance.
- Persistent pain in frail older adults increases morbidity and poor health outcomes, making treatment a priority.
- Multiple morbidity, cognitive impairment and altered pharmacokinetics and dynamics mandate an individual approach. Some basic bloodwork, including renal function, may be appropriate in the initial assessment phase and intermittently if the use of medication persists.
- As cognition worsens, pain is less likely to be reported and may manifest as other distress behaviours (e.g., agitation, resisting care, insomnia, poor appetite).
- Older adults are more likely to be taking multiple medications (polypharmacy) and have co-morbidities. , Therefore, assess individual patients for drug and disease interactions when prescribing NSAIDs and other medications.
- Risk of falls is elevated. However, pain and decreased attention or poor sleep due to chronic pain can also increase the risk of falls. Monitoring the increased risk for managing pain in the elderly is necessary to reduce suffering and increased function.
References
- Canada H. Canadian Pain Task Force Report: March 2021 [Internet]. 2021 [cited 2021 Jun 17]. Available from: https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2021.html.
- Schopflocher D, Taenzer P, Jovey R. The prevalence of chronic pain in Canada. Pain Res Manag. 2011 Dec;16(6):445–50.
- Centre for Effective Practice. (Updated May 2018). Management of Chronic Non-Cancer Pain (CNCP): Ontario. Toronto: Centre for Efective Practice.
- Ccfp CK, Perry D, Ton J, Ccfp MRK, Ccfp SG, BScPharm BT, et al. Managing opioid use disorder in primary care. :10.
- Kendall NAS, Linton SJ, Main C. Psychosocial Yellow Flags for acute low back pain: ‘Yellow Flags’; as an analogue to ‘Red Flags’; Eur J Pain. 1998 Mar;2(1):87–9.
- Hruschak V, Cochran G. Psychosocial predictors in the transition from acute to chronic pain: a systematic review. Psychol Health Med. 2018;23(10):1151–67.
- Olson KA, PhD. Pain and Sleep: Understanding the Interrelationship [Internet]. Practical Pain Management. [cited 2021 Jan 15]. Available from: https://www.practicalpainmanagement.com/pain/other/co-morbidities/pain-sleep-understanding-interrelationship
- Pain and Sleep: Common Sleep Disturbances & Tips [Internet]. Sleep Foundation. [cited 2021 Jan 15]. Available from: https://www.sleepfoundation.org/physical-health/pain-and-sleep.
- Spiegel DR, Shaukat AM, Mccroskey AL, Chatterjee A, Ahmadi T, Simmelink D, et al. Conceptualizing a subtype of patients with chronic pain: The necessity of obtaining a history of sexual abuse. Int J Psychiatry Med. 2016;51(1):84–103.
- Zis P, Daskalaki A, Bountouni I, Sykioti P, Varrassi G, Paladini A. Depression and chronic pain in the elderly: links and management challenges. Clin Interv Aging. 2017;12:709–20.
- Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, et al. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA. 2018 Mar 6;319(9):872–82.
- Rieb LM, Norman WV, Martin RE, Berkowitz J, Wood E, McNeil R, et al. Withdrawal-associated injury site pain (WISP): a descriptive case series of an opioid cessation phenomenon. Pain. 2016;157(12):2865–74.
- Rivat C, Ballantyne J. The dark side of opioids in pain management: basic science explains clinical observation. Pain Rep [Internet]. 2016 Sep 8 [cited 2020 Nov 24];1(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5741356/.
- Apkarian AV, Neugebauer V, Koob G, Edwards S, Levine JD, Ferrari L, et al. Neural mechanisms of pain and alcohol dependence. Pharmacol Biochem Behav. 2013 Nov;112:34–41.
- Baiamonte BA, Valenza M, Roltsch EA, Whitaker AM, Baynes BB, Sabino V, et al. Nicotine dependence produces hyperalgesia: role of corticotropin-releasing factor-1 receptors (CRF1Rs) in the central amygdala (CeA). Neuropharmacology. 2014 Feb;77:217–23.
- Egli M, Koob GF, Edwards S. Alcohol dependence as a chronic pain disorder. Neurosci Biobehav Rev. 2012 Nov;36(10):2179–92.
- Rieb LM, DeBeck K, Hayashi K, Wood E, Nosova E, Milloy M-J. Withdrawal-associated injury site pain prevalence and correlates among opioid-using people who inject drugs in Vancouver, Canada. Drug Alcohol Depend. 2020 Nov 1;216:108242.
- Associations between Heat Pain Perception and Opioid Dose among Patients with Chronic Pain Undergoing Opioid Tapering. :12.
- Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017 Jul;25(3):160–8.
- Mistiaen P, van Osch M, van Vliet L, Howick J, Bishop FL, Di Blasi Z, et al. The effect of patient-practitioner communication on pain: a systematic review. Eur J Pain. 2016 May;20(5):675–88.
- Van der Kolk BA, Ducey CP. The psychological processing of traumatic experience: Rorschach patterns in PTSD. J Trauma Stress. 1989;2(3):259–74.
- Trauma-Informed Practice Guide [Internet]. 2013 [cited 2019 Nov 14]. Available from: http://bccewh.bc.ca/wp-content/uploads/2012/05/2013_TIP-Guide.pdf.
- Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update [Internet]. Agency for Healthcare Research and Quality (AHRQ); 2020 Apr [cited 2021 May 5]. Available from: https://effectivehealthcare.ahrq.gov/products/noninvasive-nonpharm-pain-update/research.
- Brain K, Burrows TL, Rollo ME, Chai LK, Clarke ED, Hayes C, et al. A systematic review and meta-analysis of nutrition interventions for chronic noncancer pain. J Hum Nutr Diet. 2019 Apr;32(2):198–225.
- Rondanelli M, Faliva MA, Miccono A, Naso M, Nichetti M, Riva A, et al. Food pyramid for subjects with chronic pain: foods and dietary constituents as anti-inflammatory and antioxidant agents. Nutr Res Rev. 2018 Jun;31(1):131–51.
- Guo R, Chen L-H, Xing C, Liu T. Pain regulation by gut microbiota: molecular mechanisms and therapeutic potential. Br J Anaesth. 2019 Nov 1;123(5):637–54
- Cheatle MD, Foster S, Pinkett A, Lesneski M, Qu D, Dhingra L. Assessing and Managing Sleep Disturbance in Patients with Chronic Pain. Anesthesiol Clin. 2016 Jun 1;34(2):379–93.
- Jafari H, Courtois I, Van den Bergh O, Vlaeyen JWS, Van Diest I. Pain and respiration: a systematic review. PAIN. 2017 Jun;158(6):995–1006.
- Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing--an experimental study. Pain Med Malden Mass. 2012 Feb;13(2):215–28.
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann Behav Med. 2017 Apr;51(2):199–213.
- Majeed MH, Ali AA, Sudak DM. Mindfulness-based interventions for chronic pain: Evidence and applications. Asian J Psychiatry. 2018 Feb;32:79–83.
- Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017 14;1:CD011279.
- Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, et al. Aquatic exercise training for fibromyalgia. Cochrane Musculoskeletal Group, editor. Cochrane Database Syst Rev [Internet]. 2014 Oct 28 [cited 2019 Oct 1]; Available from: http://doi.wiley.com/10.1002/14651858.CD011336.
- Bidonde J, Busch AJ, Schachter CL, Webber SC, Musselman KE, Overend TJ, et al. Mixed exercise training for adults with fibromyalgia. Cochrane Musculoskeletal Group, editor. Cochrane Database Syst Rev [Internet]. 2019 May 24 [cited 2019 Oct 1]; Available from: http://doi.wiley.com/10.1002/14651858.CD013340.
- Bidonde J, Busch AJ, Schachter CL, Overend TJ, Kim SY, Góes SM, et al. Aerobic exercise training for adults with fibromyalgia. Cochrane Musculoskeletal Group, editor. Cochrane Database Syst Rev [Internet]. 2017 Jun 21 [cited 2019 Oct 1]; Available from: http://doi.wiley.com/10.1002/14651858.CD012700
- Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018 17;4:CD010842. .
- Chronic Pain and exercise, Exercise Is Medicine Australia Factsheet, 2014, https://exerciseismedicine.org.au/wp-content/uploads/2020/05/EIM-FactSheet_Chronic-Pain_Public.pdf.
- Nielsen A, Wieland LS. Cochrane reviews on acupuncture therapy for pain: A snapshot of the current evidence. EXPLORE. 2019 Nov 1;15(6):434–9..
- Acupuncture for neuropathic pain in adults [Internet]. [cited 2020 Dec 9]. Available from: /CD012057/SYMPT_acupuncture-neuropathic-pain-adults.
- Lee MS, Ernst E. Acupuncture for pain: an overview of Cochrane reviews. Chin J Integr Med. 2011 Mar;17(3):187–9..
- Acupuncture for Chronic Non-Cancer Pain: A Review of Clinical Effectiveness, Cost Effectiveness and Guidelines [Internet]. CADTH.ca. 2019 [cited 2021 May 5]. Available from: https://www.cadth.ca/acupuncture-chronic-non-cancer-pain-review-clinical-effectiveness-cost-effectiveness-and-0.
Practitioner Resources
- PathwaysBC: An online resource that allows GPs, nurse practitioners and their office staff to quickly access current and accurate referral information for specialists and specialty clinics, including wait times and areas of expertise. in addition, Pathways makes available hundred of patient and physician resources that are categorized and searchable. Pain Management resource video at Pathways is available at vimeo.com/528999461
- PharmaNet: PharmaNet, administered by the Ministry of Health, was developed in consultation with health professionals and the public to improve prescription safety and support prescription claim processing
- CareConnect: Secure, view-only Electronic Health Record (EHR) that delivers patient-centric information to support healthcare providers in their delivery of patient care.
- Rapid Access to Consultative Expertise (RACE) line: Pain is not listed as a specific speciality area, however, consider a RACE consult to a specialist if the pain is related to a specific specialty area. There is a provincial line for Addictions Medicine that can respond to questions related to co-occurring pain and opioid use disorder. Specialist Pain Clinics (Health Authority and Private clinics) can be found on Pathways.
- Rural Coordination Centre of BC: Real Time Virtual Support (RTVS) pathways enhance health equity in rural, remote, and First Nations communities across B.C. by connecting rural healthcare providers and patients to RTVS Virtual Physicians via Zoom or telephone. There are two types of pathways—those for healthcare providers, and those for patients. For support with myofascial pain: Quick Reply pathway for providers (myoLIVE) is available for rural and remote practitioners and clinicians who are challenged by a myofascial pain presentation.
- The Centre for Effective Practice (CEP), is an excellent resource for primary care clinicians. There is a specific link to CNCP as well as mechanical back pain - Clinically Organized Relevant Exam (CORE) Back Tool.
- First nation Health Authority – Wellness. This website lists the framework and resources to achieve a healthy lifestyle are available.
- WorkSafeBC Physician’s Hotline: Call 1-855-476-3049 to speak with an agent about access to WorkSafeBC funded programs including the following: Occupational Rehabilitation (OR1 and 2); Pain and Medication Management Program (PMMP); Resiliency over perceived trauma (ROPT); Community Pain and Addiction Services (CPAS).
- ICBC Claims: Includes information and resources related to injuries from a car crash.
- Pain BC: has several resources to support patients and caregivers, education for health professionals caring for those with pain. Some resources include Pain BC’s Live Plan Be, Chronic Pain Road Map, support line.
- Self-Management BC is part of University of Victoria’s Institute on Aging & Lifelong Health and is supported by the Patients as Partners Initiative (Primary Care Division, B.C. Ministry of Health). It offers three peer-delivered chronic pain programs free to B.C. residents.
Resources for Patients
- Pain BC: has several resources to support patients and caregivers, education for health professionals caring for those with pain. Some resources include Pain BC’s Live Plan Be, Chronic Pain Road Map, support line.
- Self-Management BC is part of University of Victoria’s Institute on Aging & Lifelong Health and is supported by the Patients as Partners Initiative (Primary Care Division, B.C. Ministry of Health). It offers three peer-delivered chronic pain programs free to B.C. residents.
- HealthLinkBC offers resources on Pain Control—Learn about pain control. At any time of the day or night, every day of the year, anyone can call 8-1-1 to be connected with a health service navigator. They provide health information, help navigate the health care system and find health services across the province, or connect with a registered nurse, registered dietitian, qualified exercise professional, or pharmacist. Registered nurses at HealthLink BC can help with non-emergency health concerns, to discuss symptoms and procedures, and to recommend whether a health care provider should be seen in person.
- Wellness Together Canada basic wellness information, to one-on-one sessions with a counsellor, to participating in a community of support.
- Work Wellness and Disability Prevention Institute aims to share the latest research and information on work wellness and disability prevention.
- Bounce Back is a free on-line service produced by the Canadian Mental Health Association-CMHA, providing assistance for those with “depression, anxiety, stress and worry”.
- AnxietyBC/heretohelp has resources to help people live well and better prevent and manage mental health and substance use problems.
- Cognitive Behavioural Therapy (CBT) Skills Groups are open to all BC residents with a valid Canadian health card number. The course is designed for adult patients (17.5 years and up) who want to learn practical tools to improve their mental health. All groups are facilitated by trained physicians.
- Cognitive Behavioral Therapy for Insomnia-CBTi, is a strategy for patients with insomnia. There are a number of practitioners and organizations that provide this service. A good initial resource from Dalhousie University is MySleepWell.
- Several YouTube videos on pain are available including: Explain pain in 5 minutes, What is chronic pain?, Why things hurt?, Pain, Is it all in your mind?, Treating Pain Using the Brain.
- Self Management Apps to put your mind in this sleep-inducing state
- mySleepButton - to put your mind in this sleep-inducing state
- MindShift - anxiety management app
- Woebot - app to support mental health
- Calm.com - app for Sleep, Meditation and Relaxation
- Curable - app for chronic pain self-care
- Curable app “an online pain psychology program. The entire program takes place online via a personal computer, tablet device, or smartphone and is delivered via a virtual pain coach.”
Appendices
- Appendix A - Overarching Considerations of Pain Management (PDF, 117KB)
- Appendix B - Non-pharmacological Treatment Modalities for Pain (PDF, 102KB)
- Appendix C - Allied Health Professionals to Support Pain Management (PDF, 96KB)
- Associated Document - List of Contributors (PDF, 73KB)
This guideline is based on scientific evidence current as of the Effective Date.
This guideline was developed by the Guidelines and Protocols Advisory Committee and adopted by the Medical Services Commission.
For more information about how BC Guidelines are developed, refer to the GPAC Handbook available at BCGuidelines.ca: GPAC Handbook.
THE GUIDELINES AND PROTOCOLS ADVISORY COMMITTEE
|
The principles of the Guidelines and Protocols Advisory Committee are to:
Contact Information: Guidelines and Protocols Advisory Committee Disclaimer The Clinical Practice Guidelines (the "Guideline") have been developed by the Guidelines and Protocols Advisory Committee on behalf of the Medical Services Commission. The Guidelines are intended to give an understanding of a clinical problem, and outline one or more preferred approaches to the investigation and management of the problem. The Guidelines are not intended as a substitute for the advice or professional judgment of a health care professional, nor are they intended to be the only approach to the management of clinical problem. We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. If you need medical advice, please contact a health care professional. |


 TOP
TOP