12 - Neurological disorder - CCMTA Medical Standards
Neurological disorders and medical fitness to drive.
12.1 About neurological disorders
Neurological disorders can affect the brain, spinal cord, nerves and muscles. They can affect an individual’s ability to think, see, communicate, move, and sense and coordinate movements. While any number of conditions fall within the category of neurological disorders, this chapter focuses on three common disorders: multiple sclerosis, Parkinson’s disease and cerebral palsy.
Multiple sclerosis
Multiple sclerosis (MS) is believed to be an autoimmune disorder in which the immune system attacks specific structures of the central nervous system (brain and spinal cord), resulting in inflammation, demyelination and axonal damage. Myelin is an essential insulation sheath of the nerve processes (axons). If it is damaged, signal transmission is slowed. Demyelination can ultimately result in permanent axonal damage in the form of scars and is called gliosis.
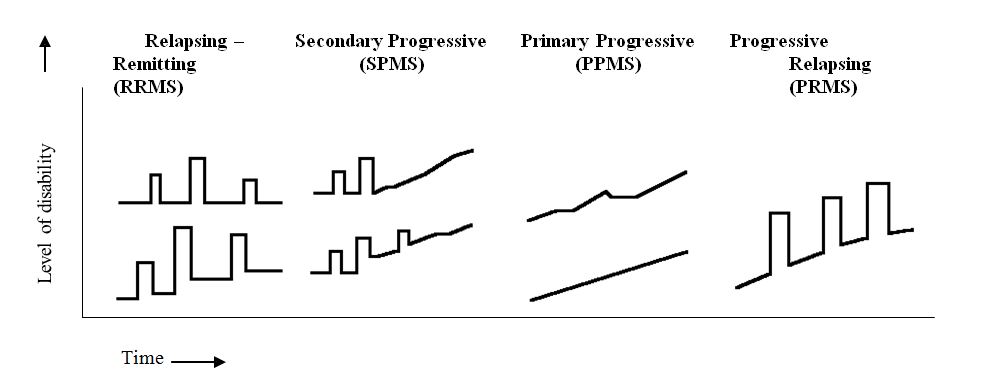
MS has an unpredictable and chronic course, leading to numerous physical and cognitive impairments. The cause is unknown. There are four clinical types of MS:
- Relapsing – Remitting (RRMS)
- Secondary Progressive (SPMS)
- Primary Progressive (PPMS), and
- Progressive Relapsing (PRMS)
Relapsing – Remitting (RRMS)
It is estimated that 55% of individuals with MS have RRMS. It is characterized by unpredictable attacks (relapses) followed by periods of months to years with no new clinical signs of disease activity (remissions). Impairments suffered during relapses may either resolve or become permanent. Approximately 10% of those with RRMS have “benign MS,” where impairments usually completely resolve between relapses and no disability is present after 10 years of disease onset. The longer a person has MS, the greater the probability that the relapses will not completely resolve and they will experience increasing disability.
RRMS accounts for over 90% of initial diagnoses of MS, but in many cases a different type emerges as the disease progresses. Approximately 50% of individuals with RRMS will eventually progress to Secondary Progressive MS within 10 years of disease onset.
Secondary Progressive (SPMS)
It is estimated that 30% of individuals with MS have SPMS. It is characterized by an initial presentation as RRMS, transitioning to a gradual progression of disability with or without superimposed relapses and minor remissions. Relapses may include new neurologic symptoms or worsening of existing symptoms. Of all the types of MS, SPMS causes the greatest amount of disability
Primary Progressive (PPMS)
It is estimated that 10% of individuals with MS have PPMS. It is characterized by a gradual progression of disability with no relapses and minor remissions from onset. The spinal cord is the area of the central nervous system primarily affected; therefore, cognitive impairments are unusual.
Progressive Relapsing (PRMS)
It is estimated that 3% to 5% of individuals with MS have PRMS. PRMS is characterized by a steady progression of disability with superimposed relapses and remissions. There may be significant recovery immediately following a relapse, but between relapses there is a gradual worsening of symptoms.
The following illustration compares the course of disability over time for each of the four types of MS.*
(*Source: The Multiple Sclerosis Information Trust, http://www.mult-sclerosis.org.)
Parkinson's disease
Parkinson’s disease (PD) belongs to a group of conditions called motor system or movement disorders, which result from the slowly progressive loss of dopamine- producing brain cells. The lack of dopamine, a neurotransmitter, interferes with the transmission of messages from the brain to nerve cells that control muscle movement and coordination. It can result in motor impairment (tremor or rigidity), and in later stages, in cognitive or autonomic dysfunction. PD is chronic and progressive, and while the specific cause is unknown, it is believed that both genetic and environmental factors contribute to the development of the disease.
Cerebral palsy
Cerebral palsy refers to any one of a number of neurological disorders that appear in infancy or early childhood and are the result of damage to, or impaired development of, the motor centres of the brain. It is a non-progressive disorder that permanently affects body movement and muscle coordination.
12.2 Prevalence
Multiple sclerosis
The prevalence of MS in Canada is among the highest in the world, with studies reporting prevalence rates from 55 to 240 per 100,000. A recent study using data from the 2001 Canadian Community Health Survey reported an overall weighted estimate of 240 per 100,000 adults (0.24%).*
(*Weighted estimate means that the results from the data are adjusted (weighted) from the sampling design using national population data.)
MS is twice as likely to affect women as men, with the highest incidence occurring in individuals in their late 30s, and the highest prevalence among those in their 40s and 50s.
Parkinson’s disease
Estimated prevalence rates for Parkinson’s disease vary widely depending on the population sampled and the methodology used. Age-adjusted prevalence rates in Canada have been reported as 125 per 100,000 (1.25%).
Cerebral palsy
The prevalence of cerebral palsy (CP) in Canadian infants is approximately 2 in 1000, with over 50,000 Canadians currently living with the disorder. The number of individuals with CP has risen slightly over the past 30 years due to higher survival rates of affected newborns as care and treatment have improved.
12.3 Neurological disorders and adverse driving outcomes
Multiple sclerosis
The research on MS and driving is limited. The results of this research indicate that driving performance may be impaired by functional deficits, including cognitive impairment, caused by MS.
Parkinson’s disease
There is a small but consistent body of research indicating that functional deficits associated with Parkinson’s disease or its treatment may impair driving performance.
Cerebral palsy
There has been no research on the effects of cerebral palsy and driving outcomes.
12.4 Effect on functional ability to drive
| Condition | Type of driving impairment and assessment approach | Primary functional ability affected | Assessment tools |
|
Multiple sclerosis Parkinson’s disease Cerebral palsy |
Persistent impairment: Functional assessment | Variable – cognitive, motor or sensory |
Medical assessments Functional assessment |
Multiple sclerosis
MS can affect motor, visual and cognitive functioning. The major symptoms associated with MS that may affect driving are:
- Ataxia (wobbliness, incoordination and unsteadiness)
- Impaired proprioception (ability to perceive the body’s position in space)
- Spasticity (involuntary muscle spasms)
- Muscle weakness
- Fatigue
- Chronic pain
- Vision problems, and
- Cognitive impairment
Vision problems are common, affecting up to 80% of individuals with MS at some point. Visual symptoms associated with MS include:
- Nystagmus (rapid, involuntary eye movement)
- Diplopia (double vision)
- Blurred vision
- Scotoma (abnormal blind spot), and
- Diminished contrast sensitivity
Cognitive impairment, particularly associated with information processing speed, is also common, affecting between 45% and 65% of those with the disease.
Medications used to treat MS that may affect driving include:
- Corticosteroids
- NSAIDS
- Antiepileptics
- Antidepressants
- Antispasticity drugs, and
- Opioids
See Chapter 15, Drugs, Alcohol and Driving for more information on these medications.
Parkinson’s disease
PD can affect motor, visual and cognitive functioning. Common motor symptoms include:
- Tremor
- Rigidity
- Bradykinesia/akinesia (slowness or absence of movement/rapid repetitive movements), and
- Postural instability
Visual impairments such as contrast sensitivity, diplopia (double vision) and impaired eye movement are sometimes seen in PD and related movement disorders. Cognitive symptoms may include:
- Psychiatric conditions such as depression, impulse control disorders and psychosis
- Sleep disturbances
- Psychomotor slowing (slow response and reaction time)
- Cognitive impairment, and
- Dementia
In addition to the symptoms noted above, fatigue and sleep disturbances are common in those with PD.
The symptoms of PD are often treated with medications including levodopa, dopamine agonists and MAO-B inhibitors. These medications can cause side effects including sleepiness, sleep attacks (sudden, overwhelming sleepiness with little or no warning signs) and visual hallucinations, which may affect driving.
A further consideration for driving is the fluctuation in the effects of medication. Individuals with advanced PD may experience periods of reduced symptom control (wearing off) near the time of their next dose of medication.
Cerebral palsy
CP can affect motor, visual, and cognitive functioning. The primary effects of CP are:
- Ataxia (wobbliness, incoordination and unsteadiness)
- Weakness and spasticity (involuntary muscle spasms), and
- Altered muscle tone that is either too stiff or too floppy
CP can also cause a loss of visual acuity or slowed visual tracking, as well as cognitive impairments such as impaired judgment and slow processing or reaction times.
12.5 Compensation
Drivers who have experienced a persistent impairment of motor or sensory function may be able to compensate. An occupational therapist, driver rehabilitation specialist, driver examiner or other medical professional may recommend specific compensatory vehicle modifications or restrictions based on an individual functional assessment.
Some examples of compensatory mechanisms are shown in the following table.
| Motor impairment | Sensory (vision) impairment |
|
|
12.6 Guidlelines for assessment
12.6.1 Neurological disorder
| National Standard |
All drivers eligible for a licence if:
|
| BC Guidelines |
|
| Conditions for maintaining licence |
No conditions are required |
| Restrictions |
RoadSafetyBC will restrict an individual’s licence so that they only drive with any permitted vehicle modifications and devices required to compensate for their functional impairment. This may include one or more of the following restrictions
|
| Reassessment |
|
| Information from health care providers |
|
| Rationale | The potential functional impairments associated with neurological disorders are variable |
