Obstructive Sleep Apnea: Assessment and Management in Adults
Effective Date: September 19, 2023
Recommendations and Topics
- Scope
- Key Recommendations
- Types of Sleep Apnea
- Epidemiology
- Risk Factors
- Risks of Untreated or Undertreated OSA
- History and Physical Examination
- Testing and Referral
- Interpretation of Results
- OSA Management
- Follow-Up
- Methodology
- Resources
Scope
This guideline applies to adult patients 19 and older with suspected obstructive sleep apnea (OSA).
While sleep apnea may occur in 1-4% of children1, pediatric diagnosis and management is beyond the scope of this guideline. For a brief pediatric overview, see Appendix A: Sleep Apnea in Children. Other conditions that may contribute to daytime sleepiness are also out of the scope of this guideline. Please see Appendix B: Other Conditions Associated with Daytime Sleepiness.
Key Recommendations
History
- If OSA is suspected, conduct a detailed history and a physical examination, focused on the upper airway.2
- The STOP-Bang questionnaire can be used to help determine if a patient is at increased risk of moderate to severe OSA.2
- While the most common symptom of OSA is excessive daytime sleepiness, the clinical presentation can vary. Completion of the Epworth Sleepiness Scale is recommended.2
- Patients with untreated OSA may have increased perioperative morbidity.3 Consider appropriate screening when referring patients for potential surgery (e.g. STOP-Bang Questionnaire). See also the BC Surgical Rehabilitation Toolkit for further information. [Expert opinion]
Testing and Referral
- Home Sleep Apnea Test (HSAT) should not be used to screen asymptomatic patients. HSAT is only recommended for the diagnosis of OSA in symptomatic patients who are determined to be at an increased risk of moderate-to-severe OSA, and who have no exclusion criteria (see Requisition).2
- A negative or equivocal HSAT does not exclude OSA. If an HSAT is negative, inconclusive or technically inadequate, and OSA is suspected, polysomnography is recommended.2
- BC now has a Standard Requisition for HSAT that referring practitioners are required to use.
- Symptomatic patients for which the HSAT is not the appropriate diagnostic test should be referred for a sleep disorder consultation for polysmnography.2 [Expert Opinion]
Management and Follow-up
- When assessing whether a patient should be treated, it is important to consider the severity of the symptoms, presence and severity of any comorbid disease, presence of any safety-critical occupation and the results of all sleep studies.
- OSA is a serious chronic disease that warrants regular follow-up, short-term to ensure initial compliance and response to treatment and long-term to confirm continued effectiveness.3
- Patients with OSA may be prone to drowsiness while driving. Physicians caring for these patients should be familiar with BC’s Driver Medical Fitness Information for Medical Professionals. [Expert Opinion]
- Surgery for OSA, including minimally invasive techniques to reduce tissue volume, incurs typical surgical risks. Since there may be effective medical alternatives to surgery, prior referral to a sleep disorder physician is recommended.
Types of Sleep Apnea
There are four types of sleep apnea:
- Obstructive sleep apnea (OSA) is the most common type of sleep apnea encountered in primary care. It is characterized by complete cessation or transient reduction in breathing with maintained or increasing respiratory effort. Home Sleep Apnea Testing (HSAT) should only be performed on patients who present with an increased risk of moderate-to-severe OSA.
- Other less common types of sleep apnea include:
- Central sleep apnea is characterized by complete cessation or transient reduction in breathing with absent respiratory effort. This occurs in patients with neurological disease or in association with drug/substance abuse or high altitude.
- Cheyne-Stokes breathing is characterized by a crescendo-decrescendo pattern of respiration between central apnea. This frequently occurs in patients with heart failure or cerebrovascular disease.
- Complex sleep apnea is characterized by the persistence or emergence of central apneas or hypopneas when treated with Continuous Positive Airway Pressure (CPAP or BiPAP) and obstructive apnea has been resolved. This may occur in up to 10% of patients with OSA treated with CPAP.
Sleep hypoventilation is a sleep disorder characterized by significant hypercapnia and hypoxemia during sleep. This usually occurs in patients with OSA and morbid obesity or obstructive or restrictive lung disease. These patients usually require urgent evaluation.4
Epidemiology
OSA is associated with poor quality of life 6,8,9 and has been linked to severe chronic health conditions such as obesity, diabetes, metabolic syndrome 3,10 and neuro-psychiatric problems. 10
Moderate–severe OSA is associated with an increased risk of cardiovascular disease, resulting in hypertension, coronary disease, stroke, heart failure, and atrial fibrillation.5
OSA is widely underdiagnosed; 86% to 95% of individuals found in population surveys with clinically significant OSA report no prior OSA diagnosis.6
The Canadian Health Measures Survey results from 2016 and 2017 showed:7
- 6.4% of Canadian adults had been diagnosed with OSA by a health care professional
- Those at particular risk include:
- Older adults (60 to 79 years, 3 times more likely)
- Males (2 times more likely to be diagnosed compared to females)
- Males reporting snoring, trouble breathing or high neck circumference (≥17 inches)
- Females reporting fatigue, insomnia, or high body mass index (>35kg/m2)
At the clinically relevant Apnea Hypopnea Index (AHI) level of 15 or greater per hour, the prevalence of OSA in the elderly population can be very high - up to 49% in some studies.8,9
Risk Factors10
Risk factors for OSA include, but are not limited to:
- Down syndrome11
- family history of obstructive sleep apnea
- Mandibular hypoplasia (retrognathia, micrognathia)
- low-lying soft palate (i.e., high Mallampati Score)
- large tongue
- tonsillar hypertrophy
- upper body obesity with a large neck size
- East Asian origin12
- Parkinson’s disease13
- traumatic brain injury14
- nasal and nasopharyngeal obstruction15
- neuromuscular disease16
- Marfan syndrome17
- polycystic ovarian disease18
Risks of Untreated or Undertreated OSA 2,19-21
Untreated or undertreated OSA pose serious risks and have been associated with: daytime sleepiness, impaired quality of life, motor vehicle crashes, occupational injury, systemic hypertension, type 2 diabetes, cardiac arrhythmia, aortic dilatation/dissection, coronary artery disease, heart failure, stroke, depression, cognitive impairment, cancer, ocular disease, pneumonia, renal dysfunction, dementia, seizures, hypogonadism, maternal/fetal health, post-operative complications, and premature death.
Patients with untreated OSA may have increased perioperative morbidity (postoperative cardiac events, acute respiratory failure, desaturation and reintubation);21 consider appropriate screening when referring patients for potential surgery (e.g. using the STOP-Bang Questionnaire, Appendix C: STOP-Bang Questionnaire). See also the BC Surgical Rehabilitation Toolkit for further information.
History and Physical Examination
- History and physical examination are crucial first steps towards the recognition and diagnosis of OSA.2 Patient history should focus on nocturnal breathing abnormalities, daytime sleepiness, and family and personal medical history.
- Consider using the STOP-Bang questionnaire to help determine if a patient is at increased risk of moderate to severe OSA (Appendix C: STOP-Bang Questionnaire).2
- Determine the patient’s risk factors for OSA (see list above).
- While the clinical presentation of OSA can vary, the most common symptom is excessive daytime sleepiness. Inquire about the impact of daytime sleepiness (e.g., “Have you had any accidents or near misses related to sleepiness while driving?” or “Have you ever had to stop an activity due to sleepiness?”). Request completion of the Epworth Sleepiness Scale. A score of greater than 10 suggests significant daytime sleepiness, although a score of 10 or less does not exclude daytime sleepiness or OSA.
- Other OSA symptoms include:
- fatigue
- habitual loud snoring
- choking, gasping, or pauses in breathing during sleep
- morning headache
- recurrent night-time awakenings
- unrefreshing or restless sleep
- impaired concentration
- nocturia
- All patients should be questioned about driving or safety critical occupation (e.g. truck, taxi, bus drivers, railway engineers, commercial pilots22) where sleepiness could be a hazard, whether they operate heavy equipment, the class of their driver’s license and whether they have fallen asleep at the wheel or have come close to doing so in the past 5 years.
Physical examination:
- Head and neck examination are important.
- Measure the neck circumference if feasible
- Examine the upper airway and it may be useful to evaluate the Mallampati score - Mallampati Classification (Appendix D: Mallampati Classification). A higher Mallampati classification has been associated with OSA diagnosis and increased AHI. For every 1- point increase in the Mallampati score, the odds of having OSA increased by more than 2-fold.23
Testing and Referral
- To determine if a patient requires a diagnostic test for OSA, it is important to first identify if they are at increased risk of moderate-to-severe OSA. This is indicated by the presence of excessive daytime sleepiness or fatigue and at least two of the following three criteria:
- witnessed apneas or gasping or choking.
- habitual loud snoring.
- diagnosed hypertension.
- If the patient is at an increased risk of moderate-to-severe OSA, then the Home Sleep Apnea Test (HSAT) is an appropriate diagnostic test, rather than a polysomnography.
- However, HSAT is not the appropriate test if one or more of the following exclusion criteria apply (any one item precludes HSAT):
- concern for non-respiratory sleep disorder (e.g., chronic insomnia, sleep walking/talking).
- risk of hypoventilation (e.g., neuromuscular disease, BMI≥ 40 kg/m2).
- chronic/regular opiate medication use.
- significant cardiopulmonary disease (e.g., history of stroke, heart failure, moderate-to-severe lung disease).
- previous negative or equivocal HSAT.
- age < 16 years.
- inability to complete necessary steps for self-administered HSAT (e.g., cognitive, physical, or other barriers).
- Recognizing that some patients may not have a bed partner, the referring physician may, while conducting a physical examination, assess whether there is a reasonable suspicion of nocturnal breathing events such as apneas, gasping, choking or habitual loud snoring.
- HSAT is not recommended for pediatric patients, however, physician evaluation, rather than age, may be the best way to determine whether an adolescent presents as an adult.
- Patients at increased risk of moderate-to-severe OSA but with one of more of the exclusion criteria above should be referred to a sleep disorder physician for potential polysomnography (PSG).
- Referral for HSAT is limited to:
- Registrants of the College of Physicians and Surgeons of British Columbia
- Nurse practitioners or other designated health professional as authorized by the College of Physicians and Surgeons of British Columbia.
- If an HSAT is negative, equivocal, or the patient has been mis-referred:
- The diagnostic facility is to notify the referring physician that the patient did not/does not meet the requirements for an HSAT and recommend a sleep disorder consultation and/or Level 1 polysomnogram study (preferred), or
- The diagnostic facility’s Medical Director or interpreting physician may refer the patient for a sleep disorder consultation and/or Level 1 study and notify the originating/referring physician, ensuring the originating/referring physician receives a copy of the HSAT result. In this case the Medical Director or interpreting physician is responsible for patient follow up as the ordering physician and cannot assume the original referring physician will provide patient follow up on the test.
Facilities must have a policy and procedure for notifying the referring physician of critical results immediately.
- To order HSAT or to request a referral for a sleep disorder consultation, see Associated Documents.
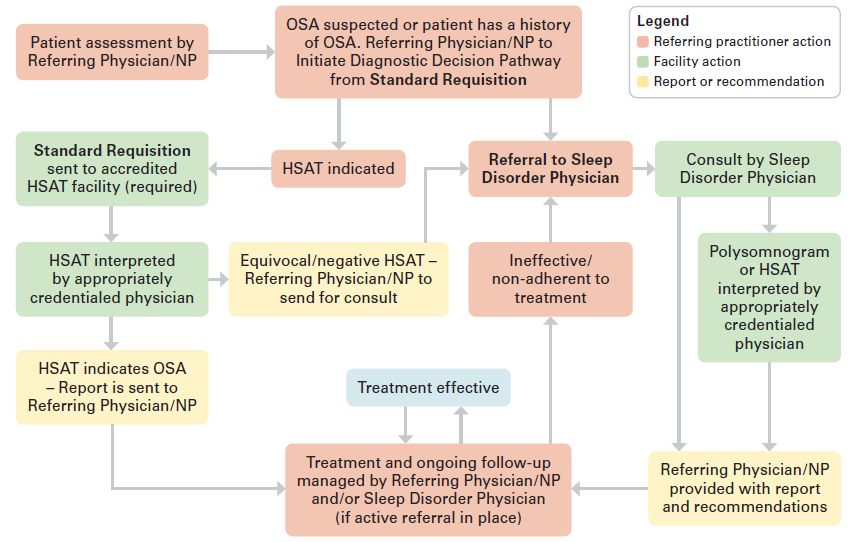
- For patients with suspected OSA, Figure 1. outlines the patient pathway.
Figure 1. Patient Pathway for Patients with Suspected OSA
Interpretation of Results
- The diagnostic sleep report should provide an assessment as to whether the patient has OSA and whether it is mild, moderate, or severe.
- Apnea Hypopnea Index (AHI) : Is defined by the number of apnea and hypopnea per hour of measured sleep.
- In addition to symptoms and presence of comorbid disease, AHI is one of the criteria used to determine the severity of sleep apnea.
AHI values should be considered in conjunction with clinical presentation, including a patient’s symptoms, co-morbidities and occupation, and all sleep monitoring abnormalities such as degree of hypoxemia (see Table 1: AHI Interpretation below).
| Result | Interpretation |
|---|---|
| AHI Values |
Severity of OSA:2 in conjunction with symptoms and comorbid disease
|
OSA Management
When assessing whether a patient should be treated it is important to consider the severity of the symptoms, presence and severity of any comorbid disease, presence of any safety-critical occupation and all the sleep monitoring abnormalities.
Patients with OSA and daytime sleepiness and/or sleep related arterial oxygen desaturation appear more likely to develop vascular complication if left untreated. It is important to treat most patients with OSA if they have comorbid disease or work in a safety critical occupation such as a commercial driver. Treatment should be considered in patients with fatigue and/or sleepiness even if the AHI is in the milder range.
Patients with OSA may be prone to drowsiness while driving. Physicians caring for these patients should be familiar with BC’s Driver Medical Fitness Information for Medical Professionals.[Expert opinion]
Surgical options are primarily for patients with tonsillar hypertrophy or craniofacial abnormalities and require referral to a sleep disorder physician and to the appropriate surgeon for more comprehensive evaluations.
Healthy Behaviours and Diet: The importance of healthy behaviours and diet, including exercise and weight loss, should be recommended for patients with elevated BMI, although it is not adequate as a stand-alone therapy if the patient is sleepy or has moderate to severe OSA. Weight loss is more successful if the patient uses definitive therapy to control their OSA and then retest after their weight goal is achieved to see if definitive therapy is still required.
Continuous Positive Airway Pressure (CPAP): CPAP is generally the most effective treatment for OSA.
If a patient is diagnosed with OSA and is unwilling or intolerant of CPAP, consider alternate therapies or refer to sleep disorder physician.
Positional Therapy: Avoiding sleeping in the supine position is an option if testing shows that OSA is primarily in the supine position. There are electronic devices that can monitor and record sleeping positions.
Other devices (oral, etc.) Oral appliances may be useful for mild to moderate OSA or those intolerant/unwilling to use CPAP and can be effective for some patients.
For additional OSA management information, see Appendix F: OSA Management Options. For additional information on oral and other devices, see Appendix G: Oral and Other Devices.
Follow-Up
- OSA is a serious chronic disease that warrants regular follow-up; short-term to ensure initial compliance and response to treatment and long-term to confirm continued effectiveness.3
- There is no need to re-test if the patient is doing well on long-term CPAP therapy and there is no change in clinical status.
- Annual follow-up is recommended with CPAP download
- Indications for retesting: Persistent daytime symptoms, abnormal overnight oximetry or residual sleep disordered breathing based on CPAP download
- Whatever treatment is used, the patient should be followed until the AHI is normal (less than 5 events per hour), the Epworth Sleepiness Scale score is 10 or less, the patient feels rested, and a bed partner reports no residual snoring. Ideally, the patient is using the treatment every night, all night.
- CPAP machines also provide a patient accessible read out of ‘events per hour’. This is an index of residual sleep apnea and not a true AHI as it is not derived from sleep monitoring but is a useful daily indication of therapy effectiveness.
Problem Solving CPAP therapy
After treatment, non-adherence to CPAP therapy, CPAP intolerance and persistent sleepiness after therapy may occur. Considerations include:
- CPAP non-adherence: Lack of interest/understanding of OSA – importance of treatment can be reinforced; depends on indications for treatment and severity of disease.24
CPAP intolerance – is common and should be addressed by the CPAP provider.24 See table below for common causes of intolerance. See Table 2: CPAP Intolerance and Treatment Recommendations below.
Table 2: CPAP Intolerance and Treatment Recommendations
| CPAP Intolerance/Problem | Recommended Treatment |
|---|---|
| Nasal congestion | Saline nasal rinses +/- intranasal steroid, increase humidity, consider full face mask |
| Difficulty exhaling against pressure | Use Expiratory Pressure Release (EPR) option |
| Mouth/nasal dryness | Adequate hydration and heated humidity on CPAP machine; chin strap for mouth leak |
| Claustrophobia | Trial of CPAP while sitting or awake and supine before using during sleep; consider nasal mask or pillows (vs full face mask) |
| Persistently elevated AHI | Make sure any leak is well controlled, obstructive events generally respond to pressure increase |
| Persistent fatigue | Ensure CPAP is used for full night (7 hours or more recommended); possible other sleep disorder, refer for consultation |
Methodology
These guideline recommendations are tailored to support practice in British Columbia and are based on the ADAPTE Collaboration guideline adaption methodology.25 Clinical recommendations were developed based on the sourced guidelines,2,3,19,26–29 a Primary Care Pathway: Uncomplicated Obstructive Sleep Apnea,24 as well as expert clinical consensus where evidence was insufficient or unavailable.
The source guidelines were chosen following an environmental scan of internationally available guidelines. Guidelines were chosen for adaptation following an evaluation using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) tool.30 In situations where there is a lack of rigorous evidence, best clinical opinion has been provided to support decision making and high-quality patient care.
The guideline development process includes significant engagement and consultation with primary care providers, sleep disorder physicians, and key stakeholders. For more information about Guidelines and Protocols Advisory Committee (GPAC) guideline development processes, refer to the GPAC handbook available at BCGuidelines.ca.
The level and quality of evidence for the key recommendations are based on those used by the AASM: Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea (2017).2 Please refer to those guidelines for a summary of the levels of evidence (table 5). Where evidence was insufficient or unavailable expert clinical consensus was used and is indicated in the key recommendations as “expert opinion”.
Resources
References
- Kirk V, Baughn J, D’Andrea L, Friedman N, Galion A, Garetz S, et al. American Academy of Sleep Medicine Position Paper for the Use of a Home Sleep Apnea Test for the Diagnosis of OSA in Children. J Clin Sleep Med. 2017 Oct 15;13(10):1199–203.
- Kapur Vishesh K., Auckley Dennis H., Chowdhuri Susmita, Kuhlmann David C., Mehra Reena, Ramar Kannan, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine. 2017;13(03):479–504.
- Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 2007 Dec 15;3(7):737–47.
- Hypoventilation syndromes - Symptoms, diagnosis and treatment | BMJ Best Practice US [Internet]. [cited 2020 Oct 26]. Available from: https://bestpractice.bmj.com/topics/en-us/1153
- Tietjens JR, Claman D, Kezirian EJ, De Marco T, Mirzayan A, Sadroonri B, et al. Obstructive Sleep Apnea in Cardiovascular Disease: A Review of the Literature and Proposed Multidisciplinary Clinical Management Strategy. JAHA [Internet]. 2019 Jan 8 [cited 2021 Jul 23];8(1). Available from: https://www.ahajournals.org/doi/10.1161/JAHA.118.010440
- Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, et al. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation [Internet]. 2021 Jul 20 [cited 2021 Jul 23];144(3). Available from: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000988
- Government of Canada SC. Sleep Apnea in Canada, 2016 and 2017 [Internet]. 2018 [cited 2021 Feb 10]. Available from: https://www150.statcan.gc.ca/n1/en/catalogue/82-625-X201800154979.
- Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015 Apr;3(4):310–8.
- Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687–98.
- Young T. Risk Factors for Obstructive Sleep Apnea in Adults. JAMA. 2004 Apr 28;291(16):2013.
- Simpson R, Oyekan AA, Ehsan Z, Ingram DG. Obstructive sleep apnea in patients with Down syndrome: current perspectives. Nat Sci Sleep. 2018;10:287–93.
- Mirrakhimov AE, Sooronbaev T, Mirrakhimov EM. Prevalence of obstructive sleep apnea in Asian adults: a systematic review of the literature. BMC pulmonary medicine. 2013 Feb 23;13:10.
- Elfil M, Bahbah EI, Attia MM, Eldokmak M, Koo BB. Impact of Obstructive Sleep Apnea on Cognitive and Motor Functions in Parkinson’s Disease. Mov Disord. 2021 Mar;36(3):570–80.
- Zuzuárregui JRP, Bickart K, Kutscher SJ. A review of sleep disturbances following traumatic brain injury. Sleep Science Practice. 2018 Dec;2(1):2.
- Michels D de S, Rodrigues A da MS, Nakanishi M, Sampaio ALL, Venosa AR. Nasal involvement in obstructive sleep apnea syndrome. Int J Otolaryngol. 2014;2014:717419.
- Albdewi MA, Liistro G, El Tahry R. Sleep-disordered breathing in patients with neuromuscular disease. Sleep Breath. 2018 May;22(2):277–86.
- Sedky K, Gaisl T, Bennett DS. Prevalence of Obstructive Sleep Apnea in Joint Hypermobility Syndrome: A Systematic Review and Meta-Analysis. J Clin Sleep Med. 2019 Feb 15;15(2):293–9.
- Kahal H, Kyrou I, Tahrani AA, Randeva HS. Obstructive sleep apnoea and polycystic ovary syndrome: A comprehensive review of clinical interactions and underlying pathophysiology. Clin Endocrinol (Oxf). 2017 Oct;87(4):313–9.
- Douglas JA, Chai-Coetzer CL, McEvoy D, Naughton MT, Neill AM, Rochford P, et al. Guidelines for sleep studies in adults – a position statement of the Australasian Sleep Association. Sleep Medicine. 2017 Aug 1;36:S2–22..
- Somboon T, Grigg-Damberger MM, Foldvary-Schaefer N. Epilepsy and Sleep-Related Breathing Disturbances. CHEST. 2019 Jul 1;156(1):172–81.
- Kaw R, Chung F, Pasupuleti V, Mehta J, Gay PC, Hernandez AV. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. British Journal of Anaesthesia. 2012 Dec 1;109(6):897–906.
- British Columbia Medical Services Commission. Policies and Guidelines of the Medical Services Commission’s Advisory Committee on Diagnostic Facilities [Internet]. British Columbia Ministry of Health; 2020. Available from: https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/medical-services-plan/diagnostic-facilities/policies_and_guidelines_of_the_acdf.pdf
- Nuckton TJ, Glidden DV, Browner WS, Claman DM. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006 Jul;29(7):903–8.
- Clinical Pathways + Specialty Access | Specialist Link [Internet]. [cited 2021 Feb 22]. Available from: https://www.specialistlink.ca/clinical-pathways/clinical-pathways.cfm
- ADAPTE Resource Toolkit for Guideline Adaptation Version 2.0 — Guidelines International Network [Internet]. [cited 2020 Mar 13]. Available from: https://g-i-n.net/document-store/working-groups-documents/adaptation/resources/adapte-resource-toolkit-guideline-adaptation-2-0.pdf/view
- Blackman A, McGregor C, Dales R, Driver HS, Dumov I, Fleming J, et al. Canadian Sleep Society/Canadian Thoracic Society position paper on the use of portable monitoring for the diagnosis of obstructive sleep apnea/hypopnea in adults. Can Respir J. 2010;17(5):229–32.
- Fleetham J, Ayas N, Bradley D, Fitzpatrick M, Oliver TK, Morrison D, et al. Canadian Thoracic Society 2011 guideline update: Diagnosis and treatment of sleep disordered breathing. Can Respir J. 2011;18(1):25–47.
- Rosen IM, Kirsch DB, Carden KA, Malhotra RK, Ramar K, Aurora RN, et al. Clinical Use of a Home Sleep Apnea Test: An Updated American Academy of Sleep Medicine Position Statement. Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 2018 15;14(12):2075–7.
- Mysliwiec V, Martin JL, Ulmer CS, Chowdhuri S, Brock MS, Spevak C, et al. The Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea: Synopsis of the 2019 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guidelines. Annals of Internal Medicine. 2020 03;172(5):325–36.
- AGREE Next Steps Consortium. The AGREE II instrument [Electronic version]. [Internet]. [cited 2020 Mar 13]. Available from: http://www.agreetrust.org
- Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012 Sep;130(3):576–84.
- Leung TN, Cheng JW, Chan AK. Paediatrics: how to manage obstructive sleep apnoea syndrome. Drugs Context. 2021;10:2020-12–5.
- Chai-Coetzer CL, Antic NA, Hamilton GS, McArdle N, Wong K, Yee BJ, et al. Physician Decision Making and Clinical Outcomes With Laboratory Polysomnography or Limited-Channel Sleep Studies for Obstructive Sleep Apnea: A Randomized Trial. Ann Intern Med. 2017 Mar 7;166(5):332–40.
- Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J Clin Sleep Med. 2019 Feb 15;15(2):301–34.
Abbreviations
AHI
BMI
CPAP
EPR
HSAT
OSA
PSG
Apnea Hypopnea Index
Body Mass Index
Continuous Positive Airways Pressure
Expiratory Pressure Release
Home Sleep Apnea Testing
Obstructive Sleep Apnea
Polysomnography
Appendices
Appendix A: Sleep Apnea in Children
Appendix B: Other Conditions Associated with Daytime Sleepiness
Appendix C: STOP-Bang Questionnaire
Appendix D: Mallampati Classification
Appendix E: Sleep Study Levels
Appendix F: OSA Management Options
Appendix G: Oral and Other Devices
Associated Documents
Referral Request – Sleep Disorder Consultation – HLTH 1945
This guideline is based on scientific evidence current as of the effective date.
The guideline was developed by the Guidelines and Protocols Advisory Committee and adopted by the Medical Services Commission.
For more information about how BC Guidelines are developed, refer to the GPAC Handbook available at BCGuidelines.ca: GPAC Handbook.
THE GUIDELINES AND PROTOCOLS ADVISORY COMMITTEE
|
The principles of the Guidelines and Protocols Advisory Committee are to:
Contact Information: Guidelines and Protocols Advisory Committee Email: hlth.guidelines@gov.bc.ca Website: www.BCGuidelines.ca Disclaimer The Clinical Practice Guidelines (the “Guidelines”) have been developed by the Guidelines and Protocols Advisory Committee on behalf of the Medical Services Commission. The Guidelines are intended to give an understanding of a clinical problem, and outline one or more preferred approaches to the investigation and management of the problem. The Guidelines are not intended as a substitute for the advice or professional judgment of a health care professional, nor are they intended to be the only approach to the management of clinical problem. We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. If you need medical advice, please contact a health care professional. |


 TOP
TOP