Anxiety and Depression in Children and Youth - Diagnosis and Treatment
This guideline was developed over 5 years ago
Recommendations and Topics
- Scope
- Diagnostic Codes
- Routine Screening and Diagnosis
- Diagnosis
- Management Considerations
- Attempt non-pharmacological management strategies first
- Treatment Algorithm for Children and Youth with Anxiety or Depression
- Treatment Type
- Medication Dosing and Follow-Up for Anxiety and Depression
- Referral to Specialist
- Rationale
- References
- Abbreviations and Terms
- Appendices
- Associated Documents
Scope
This guideline presents recommendations for early diagnosis, intervention, and maintenance treatment of depression and anxiety disorders in children and youth (18 years and under).
Diagnostic Codes
- 300 (Anxiety, dissociative and somatoform disorders)
- 308 (Acute reaction to stress)
- 311 (Depressive disorder NOS)
- 313 (Disturbance of emotions specific to childhood and adolescence)
Routine Screening and Diagnosis
Periodically screen children and youth for early signs of depression and/or anxiety. Record these results in the patient’s problem list.
Ask questions of the child (or parent where applicable) when there are red flags including: unexplained somatic complaints; unexplained behavioural changes; teenage pregnancy; school absences and family members with depression, anxiety, alcohol or other substance abuse.
Suggested questions
- Do you find yourself sad, irritable or worried a lot?
- Is the child withdrawing from or avoiding their usual activities?
Family involvement is invaluable for assisting with and monitoring treatments as well as providing assurance and emotional support for the child or youth. Assure the family that the questions and fact-finding is not to assign blame but to better understand the situation.
Choose an appropriate diagnostic questionnaire available for download on the internet. If the screen indicates a possible problem then either begin or schedule time to begin a detailed inquiry about anxiety or depressive symptoms, evaluate severity, and the potential for self-harm. Consider that there may be more than one psychiatric disorder when screening because anxiety and depressive disorders are highly comorbid in children and adolescents. Refer to Appendix A: Diagnosis of Anxiety Disorders in Children and Youth (PDF, 233KB) for descriptions of these disorders.
All youth with mood or anxiety disorders should be screened for alcohol or drug use.
Note red flags for risk of bipolar depression: family history; psychotic depression; mania with Selective Serotonin Reuptake Inhibitors (SSRIs); hyper-sexuality; risk-taking behaviour and pre-pubertal depression. Consider referral if bipolar disorder is suspected. Manage the patient while waiting for referral (see management considerations) and provide follow-up.
Diagnosis
Take a medical history and do a physical examination with attention to conditions that may mimic anxiety or depressive disorders. Consider indications for diagnostic tests such as TSH. Consider the family situation and social stressors.
Refer to Appendix A (PDF, 233KB) for descriptions of anxiety disorders, examples of anxiety disorders appearing as another disorder, prevalence, development, and treatment tips.
If post-partum depression is possible, consider referring for treatment. Manage while waiting for referral and provide follow-up.
Management considerations
Remember the basics: regular sleep, eating and exercise routines, along with consistent effective parenting are essential.1
Enlist the family for help in supporting the child with the treatment plan. Reassure them that they are not being blamed for the problems but that they can provide valuable help with developing and enacting a treatment plan and can help provide reassurance to the child or youth throughout the process. Consider the strengths of the family (and possibly larger community and school), use these and build upon them in the treatment plan.
Make a diagnosis if possible, and then begin to treat or refer as appropriate.
- Refer to Treatment Algorithm in this guideline
- Refer to Appendix A: Diagnosis of Anxiety Disorders in Children and Youth (PDF, 233KB) and Appendix B: Treatment of Anxiety Disorders and Depression in Children and Youth (PDF, 415KB)
- Provide parents with A Guide for Parents (PDF, 324KB) (either for Anxiety or Depression) and the Resource List for Families (PDF, 226KB) included with this guideline which lists pamphlets, books, web-resources and information
Set these treatment goals:
- Work towards both symptom and functional improvement including normal academic and psychosocial development
- Encourage assertiveness: taking charge of daily activities, increasing socialization, avoiding procrastination, developing goals and routines
- Teach healthy thinking: replace “what if” and self-deprecating thinking, with positive appraisals and achievable daily goals
Monitor management regularly:
- Within a week or two after initiation of treatment
- Every 2 weeks until well or is receiving secondary care
- If you are the primary care provider, then every 2 months for 6 months (as necessary)
- Structured monitoring using Appendix C: Selective Serotonin Reuptake Inhibitor (SSRI) Monitoring Form (PDF, 275KB), and Appendix D: Measurement of Functional Change (PDF, 187KB)
Avoid these common pitfalls:
- Failure to address and discourage avoidance of school, friends, work and feared situations - avoidance is instinctive and natural but unhelpful
- Allowing treatment goals to be side-tracked by physical symptoms i.e. encourage the child to continue school and activities
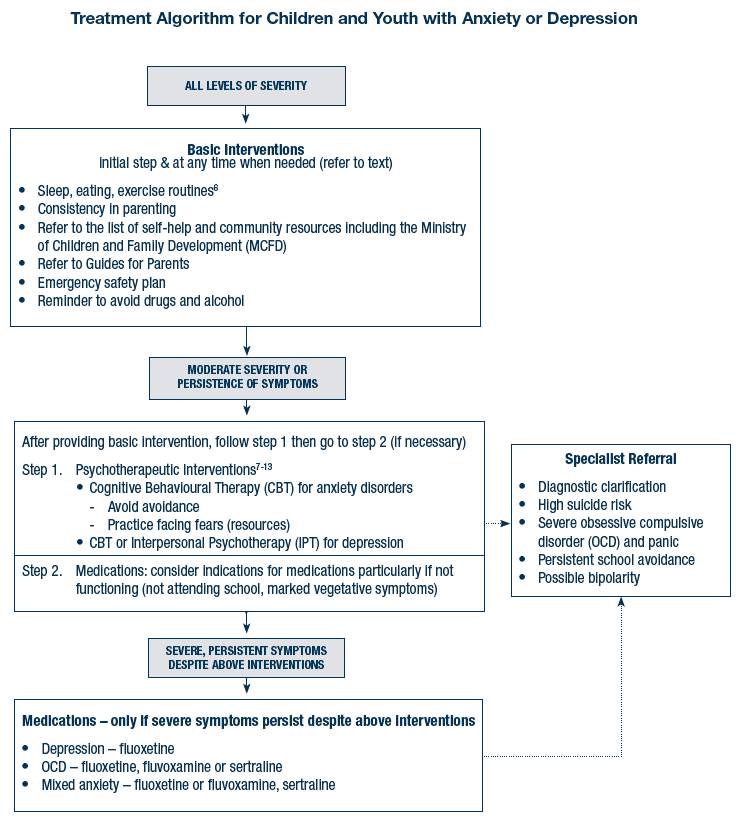
Attempt non-pharmacological management strategies first
Non-pharmacological approaches are essential first-line treatments for both anxiety2-7 and depression.2,3 It is likely that your initial visits along with parent input and books that are read by parent and child will affect a significant response.
If physician counseling, parental involvement and use of books does not effect a significant improvement it is appropriate to refer to a specialist or to the Child and Youth Mental Health team for treatment.
Treatment Algorithm for Children and Youth with Anxiety or Depression
Treatment Type
I. Cognitive Behavioural Therapy
Anxiety: The evidence-based psychological treatment for anxiety disorders is Cognitive Behavioural Therapy (CBT), a brief, directive therapy to promote realistic and adaptive thinking patterns and build behavioural competence through graduated exposure.2-7
Depression: CBT is also considered effective for child and adolescent depression.2,3
- Available through Child and Youth Mental Health teams (phone 250-387-7027 (Greater Victoria) or toll free 1-877-387-7027 or the website https://mcfd.gov.bc.ca/reporting/services/child-and-youth-mental-health or private specialists trained in CBT.
- Self-help materials based on CBT at the Anxiety Disorder Association of BC (ADABC) (phone 1-604-525-7566 or website with videos at: http://www.anxietybc.com)
- Self-help materials (e.g. “Dealing with Depression”) designed to help depressed adolescents available through the Ministry of Children and Family Development (MCFD) Child and Youth Mental Health website (https://mcfd.gov.bc.ca/reporting/services/child-and-youth-mental-health) and the Knowledge Network tool (takingcare.knowledge.ca)
There is evidence of benefit using Interpersonal Psychotherapy (IPT) but it is not as strong as for CBT.8 IPT is similar to CBT but has more focus on interpersonal problem solving. There are fewer professionals trained in IPT treatment.
- Available at some Child and Youth Mental Health teams or through some private specialists trained in IPT
II. Pharmacological Management Strategies
In general, pharmacotherapy alone is not recommended for children and adolescents. Its use should ideally be preceded and complemented by psychotherapy and/or behavioural therapy. Employ pharmacological management strategies if non-pharmacological interventions are not achieving therapeutic goals. If required, these are the issues to be considered.
There is very little peer reviewed evidence as to the safety or efficacy of SSRI medications for the treatment of anxiety and/or depression in young children. Approximately two-thirds of randomized placebo controlled pharmacological trials for depressive disorders in children and adolescents consider an age range starting from ages 6-8 through to ages 17 or 18, while the other third of cases consider ages 12/13 through 17/18.9-18
Given the above, no SSRIs are approved for marketing in Canada as appropriate medications for patients under age 18. Refer to the Health Canada statement below.21
“It is important to note that Health Canada has not approved these drugs for use in patients under 18 years. The prescribing of drugs is a physician’s responsibility. Although these drugs are not authorized for use in children, doctors rely on their knowledge of patients and the drugs to determine whether to prescribe them at their discretion in a practice called off-label use. Off-label use of these drugs in children is acknowledged to be an important tool for doctors. Doctors are advised to carefully monitor patients of all ages for emotional or behavioural changes that may indicate potential for harm, including suicidal thoughts and the onset or worsening of agitation-type adverse events.”
Adding pharmacotherapy to the non-pharmacological approaches needs to be done with careful monitoring, while informing patient and family about risks and benefit. An emergency safety plan should be made when there is moderate to severe symptoms, whether or not pharmacotherapy is used.
Indications for pharmacotherapy include: persistent depression and/or a comorbid anxiety disorder which have not responded to psychosocial interventions.
Anxiety: Drugs most often used are fluoxetine, fluvoxamine, or sertraline for Generalized Anxiety Disorder (GAD) and mixed anxiety, including social anxiety disorders and obsessive compulsive disorder (OCD). 9-14
SSRIs appear to be generally somewhat effective in randomised control trials in anxiety. Benzodiazepines are not recommended because of anger, disinhibition, habituation and irritability response.
Depression: Psychotherapy can be effective for treating depression, particularly in adolescents. If unavailable, medications may be indicated. 15-18
- The drug most often used is fluoxetine
- If bipolar vulnerability, start with a shorter-acting SSRI (e.g. sertraline)
- If comorbid anxiety, fluvoxamine or sertraline are possible alternatives
The majority of randomised control trials in depression show no significant benefit of SSRI medications over placebo. Spontaneous remission in community diagnosed adolescent depression is 50% within two months. However, those not remitting in this time period have a high risk of chronicity. Refer to a specialist.
Medication Dosing and Follow-Up for Anxiety and Depression
Initiation and Continuation: Pick target symptoms to self-monitor and document weekly (give form to parent or teenager - Appendix C (PDF, 275KB) or download from http://www.cpsbc.ca). Ask families and caregivers to help by daily monitoring the child or youth for worsening symptoms or any unusual changes or behaviours, particularly any emergence of suicidality. Discuss an emergency plan as well as planned follow-up.
General Dosing Suggestions: Start with ¼ or ½ of the adult dose and wait at least one week to increase dosages. For adolescents, the maximum dose can be similar to adults, while the dose is less than the adult dose for children.19
- Anxiety: Children who are anxious are sensitive to physical sensations. Provide support, reassurance and monitor frequently. Generalized anxiety disorder may respond at lower doses (e.g. 25-50 mg sertraline),20 OCD (100-200 mg sertraline); generally start low and increase slowly. Dosing example: 10 mg daily fluoxetine for an adolescent. For an anxious 6 year old, start with 5 mg daily and use increments of 5 mg every two weeks if needed
- Depression: The response often requires full doses for youth and the response to medication is slower. Example: start the first week with 10 mg daily of fluoxetine and increase to 20 mg daily as soon as tolerated. Increase again up 30 mg daily if not improved after 6 weeks to a maximum of 40 mg daily. If not responding after 10-12 weeks, refer to specialist.
Adverse Effects: In children, SSRIs and other new anti-depressants produce a higher rate of behavioural and emotional adverse effects (such as: agitation, disinhibition, irritability and occasionally thoughts of self-harm). The largest drug-placebo difference in the number of cases of suicidal ideation and behaviour is greatest for the under-24 age group. For all ages, the risk is highest during the first few months of drug therapy, therefore, monitor patients closely during this time. For more information, review the product monograph, Health Canada warnings for SSRIs at http://www.hc-sc.gc.ca, and the United States Food and Drug Administration (FDA) website at http://www.fda.gov.
Monitoring: Request assistance of the family and/or teenager, to monitor both symptoms and functions. Use the SSRI Monitoring Form (Appendix C (PDF, 275KB) and link below) as well as Measurement of Functional Change (Appendix D, PDF, 187KB).
Continuation: For both anxiety and depression the usual length of treatment is 6-12 months before a trial of tapering.
Discontinuation: Anxious patients are very sensitive to physical sensations during discontinuation. So, taper off particularly slowly over 1-2 months by approximately 5 mg. per reduction. For slow smooth tapering, capsules can be opened and or pills divided.
Refer to Pharmacare Plan G if financial assistance is needed for medication coverage. Information is available at Pharmacare for B.C. Residents and the form is available at https://www2.gov.bc.ca/gov/content/health.
Referral to Specialist
Indications for referral to a specialist:
- Depression or anxiety that has not responded to primary treatment
- High suicide risk
- Severe OCD and panic
- Persistent school avoidance
- Possible bipolarity
- Postpartum depression
Referral options (also refer to other resources in the Resource List for Physicians (PDF, 303KB))
- Continue to follow the patient until they are seen by the specialist.
- For specialist mental health consultation and CBT refer to MCFD - Child and Youth Mental Health (1-250-387-7027 (Greater Victoria) or toll free 1-877-387-7027); or contact a community or private Psychiatrist
- Community or private psychologist with skills in CBT for children and youth.
- British Columbia Psychological Association at 1-604-730-0522 (Lower Mainland) or toll free 1-800-730-0522 or the website https://referral.psychologists.bc.ca/
- For treatment resistant cases (aged 6 to 19), refer to the tertiary care Mood and Anxiety Disorders Clinic at BC Children’s Hospital, 1-604-875-2010 or the website at http://www.bcchildrens.ca/our-services
Rationale
Psychiatric disorders in children and youth are under-detected in health care settings. Symptoms are likely to be missed unless they are severe or accompanied by physical illness.25 Under-detection represents a serious omission given the research evidence establishing effective treatments for both anxiety and depression in children.1-18
The prevalence of anxiety disorders in children aged 5 to 17 is 6.4%.22 The debilitating nature of these disorders is routinely underestimated and the need for help may not be realized until serious impairment in social and academic functioning has occurred.23 Untreated anxiety disorders in children and adolescents are associated with higher rates of comorbid depression and substance abuse.24
Depression affects 3.5% of children at any given time, impeding healthy psychosocial development.1 Diminished self-worth, academic struggles, and difficulties in social relations with family and peers exert a heavy toll on youth who are often unable to communicate the nature of their experience. Clinical depression during adolescence represents the strongest risk factor for teenager suicide and is linked to significant psychosocial impairment in adulthood.23
Periodic screening of children presenting -- for any reason -- to primary care physicians can improve clinical recognition of these disorders and result in improved rates of treatment.26
References
- Larun L, Nordheim L, Ekeland E, et al. Exercise in prevention and treatment of anxiety and depression among children and young people (Review). Cochrane Database of Systematic Reviews 2006;3.
- Compton S, March J, Brent D, et al. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adoles Psychiatry 2004;43(8):930-59.
- Chu B, Harrison T. Disorder-specific effects of CBT for anxious and depressed youth: a meta-analysis of candidate mediators of change. Clin Child Fam Psychol Rev 2007;10:352-72.
- Kendall P, Brady E, Verduin T. Comorbidity in childhood anxiety disorders and treatment outcomes. J Am Acad Child Adolesc Psychiatry 2001;40(7):787-794.
- Soler J, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database of Systematic Reviews 2005;4.
- O’Kearney R, Anstey K, von Sanden C. Behavioural and cognitive behavioural therapy for obsessive compulsive disorder in children and adolescents. Cochrane Database of Systematic Reviews 2006;4.
- Lumpkin P, Silverman W, Weems C, et al. Treating a heterogeneous set of anxiety disorders in youths with group cognitive therapy: A partially non concurrent multiple-baseline evaluation. Behavior Therapy 2002;33(1):163–77.
- Mufson L, Dorta K, Wickramaratne P, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 2004;61:577–84.
- Stein D, Ipser J, van Balkom A. Pharmacotherapy for social anxiety disorder. Cochrane Database of Systematic Reviews 2000;4.
- Kapczinski F, Lima M, Souza J, et al. Antidepressants for generalized anxiety disorders. Cochrane Database of Systematic Reviews 2003;2.
- Hawkridge S, Ipser J, Stein D. Pharmacotherapy for anxiety disorders in children and adolescents (Protocol). Cochrane Database of Systematic Reviews. 2005;1.
- Geller D, Biederman J, Mullin B, et al. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am J Psychiatry 2003;160(11):1919-28.
- Clark D, Birmaher B, Axelson D, et al. Fluoxetine for the treatment of childhood anxiety disorders: open-label, long-term extension to a controlled trial. J Am Acad Child Adolesc Psychiatry 2005; 44(12):1263-1270.
- The Research Unit on Pediatric Psychopharmacology Anxiety Study Group. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. NEJM 2001;344(17):1279-85.
- Hughes C, Emslie G, Crismon M, et al. Texas children’s medication algorithm project: update from Texas consensus conference panel on medication treatment of childhood major depressive disorder. J Am Acad Child Adolesc Psychiatry 2007;46(6):667-86.
- Hetrick S, Merry S, McKenzie J, et al. Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents. Cochrane Database of Systematic Reviews 2007;3.
- Cheung A, Emslie G, Mayes T. Review of the efficacy and safety of antidepressants in youth depression. Child Psychol Psychiatry 2005;46(7):735-54.
- Donnelly C, Wagner K, Rynn M, et al. Sertraline in children and adolescents with major depressive disorder. J Am Acad Child Adolesc Psychiatry 2006;45(10):1162-70.
- Canadian Pharmacists Association. Compendium of pharmaceuticals and specialties. Ottawa: Canadian Pharmacists Association; 2008.
- Rynn M, Siqueland L, Rickels K. Placebo-controlled trial of sertraline in the treatment of children with generalized anxiety. Am J Psychiatry 2001;158(12):2008-14.
- Health Canada. Advisory: Health Canada advises Canadians of stronger warnings for SSRIs and other newer anti-depressants. 2004. Available at http://www.hc-sc.gc.ca/dhp-mps/alt_formats/hpfb-dgpsa/pdf/medeff/prozac_hpc-cps-eng.pdf Accessed September 10, 2009.
- Waddell C, Offord D, Shepard C, et al. Child psychiatric epidemiology and Canadian public policy-making: the state of the science and art of the possible. Can J Psychiatry 2002;47:825-832.
- Roza S, Hofstra M, van der Ende J, Verhulst F. Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: a 14-year follow-up during childhood, adolescence, and young adulthood. Am J Psychiatry. 2003;160(12):2116-21.
- Lewinsohn P, Rhode J, Seeley P, et al. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. J Abnorm Psychol 2003;112(3):353-363.
- Cheung A, Zuckerbrot R, Jensen P, et al. Guidelines for adolescent depression in primary care (GLAD-PC: II). Treatment and Ongoing Management. Pediatrics 2007;120(5)e:1313-26.
- Vander Stoep A, Weiss N, McKnight B, et al. Which measure of adolescent psychiatric disorder--diagnosis, number of symptoms, or adaptive functioning--best predicts adverse young adult outcomes? J Epidemiol Community Health 2002;56(1):56-65.
List of Abbreviations
| ADABC | Anxiety Disorders Association of BC |
| CBT | Cognitive Behavioural Therapy |
| FDA | United States Food and Drug Administration |
| GAD | Generalized Anxiety Disorder |
| IPT | Interpersonal Psychotherapy |
| MCFD | Ministry of Children and Family Development |
| OCD | Obsessive compulsive disorder |
| SSRI | Selective serotonin reuptake inhibitor |
| TSH | Thyroid-stimulating hormone or thyrotropin |
Appendices
Appendix A – Diagnosis of Anxiety Disorders in Children and Youth (PDF, 324KB)
Appendix B – Treatment of Anxiety Disorders and Depression in Children and Youth (PDF, 415KB)
Appendix C – Selective Serotonin Reuptake Inhibitor (SSRI) Monitoring Form (PDF, 275KB)
Appendix D – Measurement of Functional Change in depressed and/or Anxious Patients (PDF, 187KB)
Associated Documents
The following documents accompany this guideline:
- The Full Guideline (PDF, 325KB)
- Resource Guide: Information Sources for Physicians (PDF, 303KB)
- Resource Guide: Information Sources for Families (PDF, 226KB)
- Anxiety in Children and Youth: A Guide for Parents (PDF, 324KB)
- Depression in Children and Youth: A Guide for Parents (PDF, 200KB)
|
The principles of the Guidelines and Protocols Advisory Committee are to:
|
Contact information
Guidelines and Protocols Advisory Committee
PO Box 9642 STN PROV GOVT
Victoria BC V8W 9P1
Phone: 1-250-952-1347
Fax: 250-952-1417
Email: hlth.guidelines@gov.bc.ca
Web site: www.BCGuidelines.ca