Medical Assistance in Dying - Information for Health-Care Providers
Health-care providers may have questions regarding the administrative steps in providing medical assistance in dying (MAiD) in B.C., as well as questions regarding their reporting obligations. This page contains information on some of the common administrative processes involved in providing medical assistance in dying, as well as information on the reporting requirements and provincial forms to be used for this purpose.
Reporting Requirements for Practitioners and Pharmacists
All required provincial forms for medical assistance in dying must be submitted to the B.C. Ministry of Health, the designated recipient of reportable information from physicians, nurse practitioners and pharmacists.
How to Submit
Provincial MAiD forms can be submitted to the MAiD Oversight Unit at the B.C. Ministry of Health in three different ways:
- Fax: +1 778-698-4678,
- The secure MAiD Reporting Portal, or
- Secure email hlth.maidoversight@gov.bc.ca (see BC Physician Privacy Toolkit for privacy regulations).
If you have questions about how to report or what is considered reportable information, please see below.
Physicians, nurse practitioners and pharmacists have reporting obligations that they must be aware of. These requirements are specified in the federal Regulations for the Monitoring of Medical Assistance in Dying (which have been revised, effective Jan. 1, 2023), and on this webpage.
All provincial and federal reportable information is included on B.C.’s provincial forms for medical assistance in dying. This means that the practitioner (Assessor and Prescriber) or pharmacist’s completion and submission of their provincial form(s) to the B.C. Ministry of Health will fulfill their provincial and federal reporting obligations regarding medical assistance in dying. Having a single designated recipient streamlines the reporting process for B.C. practitioners and pharmacists. (PLEASE NOTE: as a result of updated federal regulation which came into effect on January 1, 2023, the standardized provincial forms for MAiD have been updated to ensure that they include all reporting requirements under this updated regulation).
Practitioners and pharmacists must provide supplemental information to the Ministry of Health’s MAiD Oversight Unit upon request. The MAiD Oversight Unit reviews all reportable information, including every instance of MAiD provision in B.C., for completeness of reporting and compliance with the eligibility criteria, federal safeguards, provincial safeguards, and regulatory college practice standards for MAiD. If additional information is required, or if the information reported requires clarification, staff at the MAiD Oversight Unit will reach out to practitioners and pharmacists to obtain this information.
What is reportable – by who and when?
There are a number of reporting requirements for practitioners (Assessors and Prescribers) and pharmacists (see 1 to 3 below), which includes the requirement that practitioners report on deaths due to medical assistance in dying (see 4). See the Medical Assistance in Dying in British Columbia: Reporting at a Glance (PDF, 249KB) one-page reference guide.
Practitioners have reporting obligations if they receive a request for MAiD and assess the patient for eligibility even if the request does not result in medical assistance in dying.
What constitutes a request for MAiD?
A patient’s request for MAiD may be verbal or written, and may take any form (a discussion with the practitioner, an email, a text message, etc.). However, to create a reporting requirement, a request for MAiD must be an intentional or explicit request seeking MAiD. An inquiry about MAiD, such as asking for general information about MAiD eligibility or the provision of MAiD, does not constitute a request for MAiD. Similarly, a general discussion between the patient and a MAID Assessor or Prescriber on their views regarding applicability of eligibility in the case of this specific person would also not constitute an “intentional” request for MAiD for the purposes of triggering a reporting requirements.
Note: The definition above only applies to what triggers a reporting requirement and not to the actual provision of MAiD. Federal safeguards require that the patient make a written request for written request for MAiD before MAiD provision can occur, which in B.C. requires the patient’s completion of the Request for Medical Assistance in Dying (HLTH 1632) form.
- Ineligibility, withdrawal of request, or death from another cause (Practitioner)
A practitioner who receives a patient’s request for MAiD for the purpose of eligibility assessment or provision of medical assistance in dying, must report to the Ministry of Health within 30 days of becoming aware of any of the following information related to patient ineligibility or planning being discontinued:
- The patient is assessed as ineligible for MAiD;
- The patient is now ineligible after previously being assessed as eligible;
- The patient has withdrawn their request; or
- The patient has died from another cause
The Assessor will report using the Assessment Record (Assessor) form (HLTH 1633).
The Prescriber will report using the Assessment Record (Prescriber) form (HLTH 1634).
Note: The Assessor or Prescriber must include the patient's Request for Medical Assistance in Dying form (HLTH 1632) and, if applicable, the Consultant’s Assessment (HLTH 1635) with their reporting, and will fax or email the required forms to the Ministry of Health at 778 698-4678 or hlth.maidoversight@gov.bc.ca.
Reporting caveat (under the federal Regulations):
- This reporting is not required if the practitioner becomes aware of the information “after the 90th day after the day on which the practitioner received the request”.
- Dispensing of substance for medical assistance in dying (Pharmacist)
The full pharmacist who dispenses a substance in connection with the provision of medical assistance in dying must report to the Ministry of Health within 6 business days of the day on which the substance is scheduled to be administered to the patient.
Reporting is accomplished by the full pharmacist completing (in collaboration with the prescribing practitioner) and faxing or emailing the Dispensing Record (Pharmacist) (HLTH 1641) form to the Ministry of Health at 778 698-4678, hlth.maidoversight@gov.bc.ca or uploading the form to our secure MAiD Reporting Portal.
- Provision of medical assistance in dying (Practitioner)
The practitioner who provides medical assistance in dying (by administering a substance or providing a substance for the patient’s self-administration) must report to the Ministry of Health within 72 hours of confirmation of the patient’s death.
The Prescriber will report using the Assessment Record (Prescriber) (HLTH 1634) form, which includes sections on the planning and administration of medical assistance in dying. The Prescriber will include the following forms with their reporting and will fax or email or upload the forms to the Ministry of Health at 778-698-4678, hlth.maidoversight@gov.bc.ca, or to our secure MAiD reporting Portal: Request for Medical Assistance in Dying (HLTH 1632); Assessment Record (Assessor) (HLTH 1633); Consultant’s Assessment (HLTH 1635) if applicable; Waiver of Final Consent (HLTH 1645) if applicable; Prescription and Medication Administration Record. These forms are also identified on the Medical Assistance in Dying in British Columbia: Reporting at a Glance (PDF, 249KB) one-page reference document.
Note 1: The Medical Certification of Death form must be completed and submitted to the funeral director so that a Disposition Permit may be issued, not to the Ministry of Health fax number for reporting on medical assistance in dying.
Note 2: As is the case with other deaths in B.C., if the patient’s underlying condition relates to an accident, violence or self-inflicted injury, the practitioner must also report the death to the coroner on call in the region where the incident giving rise to the injury occurred by calling 1 855 207-0637.
Why are some B.C. reporting timelines shorter than the federal ones?
In B.C., some of the timelines for practitioner and pharmacist reporting have been shortened compared to what are outlined in the federal Regulations. The following two shortened timelines ensure that B.C. practitioners and pharmacists only have to report once to meet provincial oversight and federal monitoring requirements:
- Provision of medical assistance in dying - the providing practitioner (Prescriber) is required to report within 72 hours of confirmation of the patient’s death (instead of “within 30 days” under the federal Regulations).
- Dispensing for medical assistance in dying - the dispensing pharmacist is required to report within 6 business days after the day on which the substance is scheduled to be administered to the patient (instead of “within 30 days” under the federal Regulations).
What forms must be completed and where can I find them?
The provincial standardized forms for medical assistance in dying are available on the Ministry of Health’s website (see quick link to Forms in right column of this page). These provincial forms are to be used by patients, practitioners and pharmacists, and must be downloaded from this website each time they are required to ensure the most recent version is used.
The set of provincial forms related to medical assistance in dying includes the following:
- Request for Medical Assistance in Dying (HLTH 1632) - for a patient to record details related to their request for medical assistance in dying.
- Waiver of Final Consent (HLTH 1645) – to record a written arrangement between the patient and MAiD prescriber waiving the requirement for the patient to give express consent immediately prior to MAiD provision.
- Assessment Record (Assessor) (HLTH 1633) - for an assessing practitioner to record details of a patient’s eligibility assessment, and, if applicable, reasons for planning being discontinued (e.g., due to a patient withdrawing their request).
- Assessment Record (Prescriber) (HLTH 1634) – for a prescribing practitioner to record details of a patient’s eligibility assessment and, if applicable, reasons for planning being discontinued or details related to the planning and administering of medical assistance in dying.
- Consultant’s Assessment of Patient’s Informed Consent Decision Capability (HLTH 1635) – for a consulting practitioner to record details of their capability assessment.
- Dispensing Record (Pharmacist) (HLTH 1641) – for a full pharmacist to record details of their dispensing and the prescribing practitioner’s receipt of medications, as well as the reconciliation of returned medications after medical assistance in dying.
- Medical Certification of Death (VSA 406A) – the prescribing practitioner must complete this form within 48 hours of death in compliance with Section 18 of the Vital Statistic Act, and provide the completed form to the funeral director so that a Disposition Permit may be issued. (This form is not to be submitted to the Ministry of Health for reporting on medical assistance in dying.)
The completion of these provincial forms meets the requirements of the federal Regulations for the Monitoring of Medical Assistance in Dying, B.C.’s professional regulatory colleges (Physicians and Surgeons, Nursing Professionals, and Pharmacists), the B.C. Ministry of Health and the B.C. Vital Statistics Agency, regarding the completion of documentation and reporting on medical assistance in dying. Please see the Forms page for access to these forms.
Where are the forms to be submitted?
The patient can submit their Request for Medical Assistance in Dying (HLTH 1632) directly to their physician or nurse practitioner, or can contact a health authority’s care coordination service for medical assistance in dying (see health authority links below).
The physician, nurse practitioner or pharmacist will fax, email or upload their requisite provincial form(s) to the Ministry of Health at 778 698-4678, hlth.maidoversight@gov.bc.ca, or to our secure MAiD Reporting portal within the timeframe required for each reporting requirement.
Note: Details on reporting requirements are addressed in the section above titled “What is reportable – by who and when?” As well, instructions are indicated at the top of each provincial form and in its accompanying instruction guide (see quick link to Forms page in right column on this page).
What is the process for prescribing drugs used in medical assistance in dying?
Physicians, nurse practitioners and pharmacists must follow the standards set out by their respective professional college when writing a prescription or dispensing drugs for medical assistance in dying. There is an expectation that the British Columbia standardized drug protocols and prescription form will be used.
The British Columbia Pharmacy Protocols guidance document and the British Columbia Medical Assistance in Dying Prescription form (includes the pre-printed order and medication administration record) are not available for general distribution. The prescribing physician or nurse practitioner can access these documents by contacting the health authority care coordination service for medical assistance in dying, or the College of Physicians and Surgeons. Pharmacists may also familiarize themselves with the standardized drug protocols by accessing the British Columbia Pharmacy Protocols guidance document through the secure portion of the College of Pharmacists website.
Since March 20, 2020, PharmaCare coverage for MAiD prescriptions is provided automatically under Assurance (Plan Z). Prescribers can simply send their prescription to the pharmacy. Pharmacists can make a claim through PharmaNet using the MAiD-specific PINs.
If a patient is ineligible for coverage of MAiD drugs because they are not enrolled in MSP -- because they recently moved to B.C. from another part of Canada -- please call HIBC.
More information on the expectations related to the prescription process is available in the standards of the College of Physicians and Surgeons, the standards, limits and conditions of the College of Pharmacists of British Columbia, and the standards, limits and conditions of the British Columbia College of Nurses and Midwives.
How do I fill out the death certificate after providing medical assistance in dying?
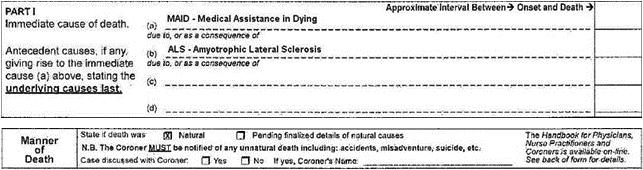
In order to meet the requirement that medical assistance in dying is indicated on the Medical Certification of Death and that the cause of death is the underlying illness or disease causing the grievous and irremediable medical condition, the Vital Statistics Agency recommends that the Medical Certification of Death be completed as follows:
- Report medical assistance in dying in PART 1 (a);
- Report the underlying illness/disease causing the grievous and irremediable medical condition in PART I (b); and
- Report manner of death as "natural."
For example:
What is the MAiD Oversight Unit and why might they contact me?
The MAiD Oversight Unit at the Ministry of Health is responsible for the monitoring, reporting, and oversight of MAiD in B.C. The MAiD Oversight Unit is the designated recipient of all federally and provincially reportable information in the province. All MAiD provisions and discontinuations in B.C. are reviewed by the MAiD Oversight Unit for compliance with eligibility criteria, federal safeguards, provincial safeguards, regulatory college practice standards, and reporting requirements for MAiD. If any required information is missing, the information provided requires clarification, or supplemental information is required, staff within the MAiD Oversight Unit will contact practitioners and pharmacists to obtain this information.
Who should I contact with questions about medical assistance in dying policy and processes?
Health-care providers working within health authorities should contact their health authority’s designated coordinator for medical assistance in dying, or their supervisor for more information on policy and processes. Health authorities play a central role in the co-ordination of medical assistance in dying services, and are prepared to support patients and care providers who need assistance in navigating the service.
Fraser Health
Interior Health
Island Health
Northern Health
Provincial Health Services Authority
Vancouver Coastal Health
Health-care providers not affiliated with a health authority should contact their provincial regulatory college for information on medical assistance in dying processes.
For people living in a First Nations community or care providers working in First Nations communities, please email the First Nations Health Authority (maid@fnha.ca) if you have any questions or require further assistance in coordination.
Standards and Guidelines
The provincial regulatory colleges have laid out medical assistance in dying standards and guidelines so registrants know what is expected of them when they are approached about or are participating in providing the service:
- Standards from the College of Physicians and Surgeons of B.C.
- Standards for nurse practitioners from the B.C. College of Nurses and Midwives
- Scope of Practice for registered nurses from the B.C. College of Nurses and Midwives
- Standards from the College of Pharmacists of B.C.
How do I bill MSP for medical assistance in dying services?
The following fees for medical assistance in dying have been approved:
P13501 MAiD Assessment Fee – Assessor Prescriber
P13502 MAiD Assessment Fee – Assessor
P13503 Physician witness to video conference MAiD Assessment – Patient Encounter
P13504 MAiD Event Preparation and Procedure
P13505 MAiD Medication Pick-up and Return
P13506 MAiD Expert Case Review*
P13507 MAiD Waiver of Final Consent*
P13508 Oral MAiD Extension*
*As of September 1st, 2023.
Information regarding specific MSP fee codes can be found on the MSC Payment Schedule webpage:
How do I bill for approved travel and training for these services?
The Medical Assistance in Dying Travel and Training Assistance Program provides funding to assist health authorities in the provision of medical assistance in dying services to residents in Rural Subsidiary Agreement communities. The program policy and forms are accessible at the following Rural Practice Programs link:
