Drug administration fee
When a pharmacist administers an eligible injection, they must claim the PharmaCare drug administration fee ($11.41). Pharmacists cannot charge the patient for the service under the Full Payment Policy — Section 5.10, PharmaCare Policy Manual. Patients must be actively enrolled in MSP.

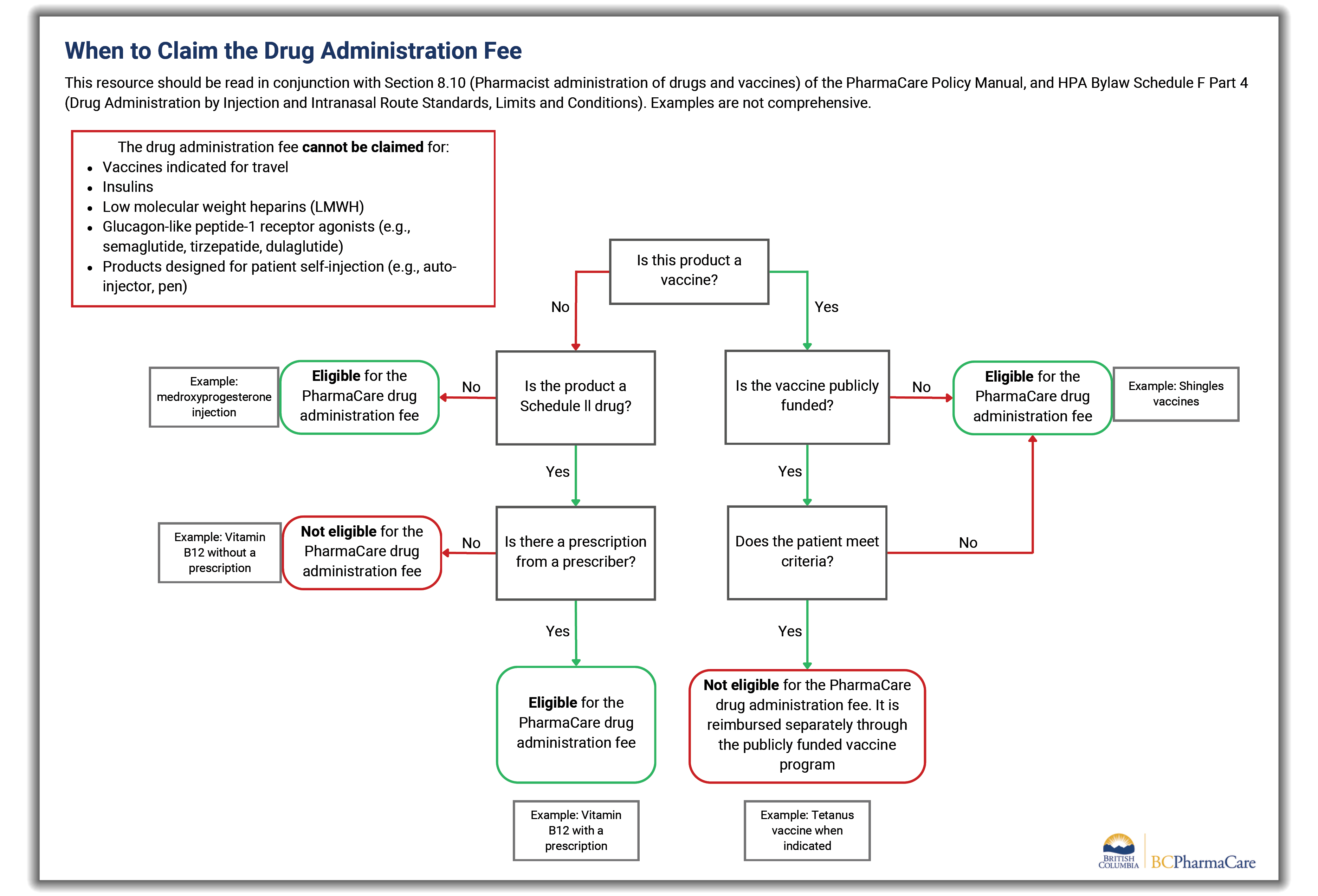
A prescription is needed for pharmacists to administer and claim the fee for Schedule II drugs (e.g., vitamin B12, dimenhydrinate). A prescription is not needed for vaccines.
The drug administration fee cannot be claimed for:
- Vaccines indicated for travel
- Insulins
- Low molecular weight heparins (LMWH)
- Glucagon-like peptide-1 receptor agonists (e.g., semaglutide, tirzepatide, dulaglutide)
- Products designed for patient self-injection (e.g., auto-injector, pen)
If a vaccine commonly used as a travel vaccine (such as hepatitis A) is administered for an indication other than travel, pharmacists must claim the drug administration fee and must not charge the patient.
For multiple injections for one patient on the same day, PharmaCare will pay the drug administration fee and dispensing fee for each injection. However, payments for injectable opioid agonist treatment (iOAT) injections are limited to 4 per patient per day. For multiple injections, use the PharmaNet intervention code UF.
The maximum PharmaCare reimburses for a combination of medication review services, clinical services, or drug administration for the same patient, on the same day, from the same pharmacy, is $78.00.
For further details, view Pharmacist administration of drugs and vaccines — Section 8.10, PharmaCare Policy Manual
PharmaNet claim procedures
The pharmacist must enter the claim in PharmaNet on the date of injection.
- Enter P1 in PractIDRef (for CPBC) and your CPBC ID for PractID
- Use PIN 66128366
- For Quantity, enter 1
- Do not enter a drug cost or fee
- In SIG field, enter DIN_generic name_route_admin site, e.g., 0273497_VitB12_IM_LEFT

Resources
- Drug administration fee flowchart (PDF, 50KB)
- PharmaCare Policy Manual:
- PharmaCare’s related services list shows pharmacy services fees
- BCCDC information about publicly funded vaccines