Genital Tract Cancers in Females: Human Papillomavirus Related Cancers (Cervical, Vaginal & Vulvar)
Effective Date: June 15, 2014
Revised Date: July 15, 2016
Recommendations and Topics
Scope
This guideline provides recommendations for the screening, diagnosis, and follow-up care of human papillomavirus (HPV) related cancers, including cervical, vaginal, and vulvar, in females aged ≥ 9 years (this age limit due to the HPV immunization recommendations).
This guideline is part of the BCGuidelines.ca – Genital Tract Cancers in Females series. The series includes two other guidelines: Endometrial Cancer and Ovarian, Fallopian Tube and Primary Peritoneal Cancers. Signs and symptoms for the different female genital tract cancers may overlap (e.g., abnormal uterine bleeding); and therefore these guidelines may need to be used in conjunction with each other when performing initial diagnostic investigations.
Key Recommendations
- HPV immunization is recommended for the prevention of HPV infection, which is the major risk factor for cervical, vaginal and vulvar cancers. 1
- Screening for cervical cancer in asymptomatic females should be offered per the BC Cancer Agency's (BCCA) Cervical Cancer Screening Program, which were updated in June 2016. 2
- If cancer of the cervix is clinically suspected, then proceed to biopsy or colposcopy - even in the case of a normal Papanicolaou smear test (Pap test) result.
Risk Factors
The major risk factor for cervical, vaginal, and vulvar cancers is HPV infection. 1,2 Additional risk factors include sexual activity at a young age, multiple sexual partners or a partner who has had multiple sexual partners, history of other sexually transmitted infections (STIs), and smoking.1-4
Prevention
Prevention of cervical, vaginal and vulvar cancers revolves around preventing HPV infection through HPV immunization and avoiding skin-to-skin sexual contact with another person through safe sexual behaviours (e.g., condom use5,6). Sexual contact may be defined as intercourse, digital or oral sexual contact involving the genital area.
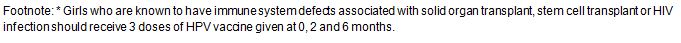
HPV Immunization Recommendations7
According to National Advisory Committee on Immunization (NACI; February 2015):
- HPV vaccine (Cervarix® or Gardasil®) is recommended for females between 9 and 26 years of age.
- HPV vaccine (Cervarix® or Gardasil®) may be administered to females > 26 years of age.
HPV Vaccines
For females aged 9 to 45 years without prior HPV exposure, both the quadrivalent (Gardasil®) and bivalent (Cervarix®) vaccines have been shown to have a positive effect for the prevention of HPV-related infection and precancerous cervical disease. However, the overall effectiveness of preventing against cervical cancer has not been demonstrated.
As the HPV vaccines do not protect against all cancers of the cervix, nor do they eliminate pre-existing infection, females should continue cervical cancer screening as per BCCA guidelines. For males, Gardasil® is the only vaccine approved for use in males aged between 9 and 26 years, but at this time there is no publicly funded HPV vaccine program in BC for males.
The two types of HPV vaccines are:
- Quadrivalent HPV vaccine (Gardasil®)7,8 – protects against HPV types 6, 11, 16, and 18
- Indications for females aged between 9 and 45 for the prevention of:
- cervical, vulvar and vaginal cancer (caused by HPV types 16 and 18);
- genital warts (condyloma acuminata; caused by HPV types 6 and 11); and
- precancerous or dysplastic lesions (caused by HPV types 6, 11, 16 and 18).
- Indications for females aged between 9 and 26 for the prevention of:
- anal cancer (caused by HPV types 16 and 18); and
- precursor lesions (caused by HPV types 6, 11, 16 and 18).
- Offered free for BC females born in 1994 or later, available through a school-based program (starting in grade 6), physician, pharmacist, or local health unit.9
- Also available for those not eligible for free HPV vaccine through patient-pay (approximately $500 for the 3 doses).
- Indications for females aged between 9 and 45 for the prevention of:
- Bivalent HPV vaccine (Cervarix®)7,10,11 – protects against HPV types 16 and 18
- Indications for females aged between 9 and 45 for the prevention of:
- cervical cancer (caused by HPV types 16 and 18); and
- precancerous or dysplastic lesions (caused by HPV types 16 and 18).
- Offered free for BC females aged ≤ 26 years and born before 1994, available through physician, pharmacist, sexual health clinic, youth clinics and student health centre. This is a time-limited program that is available while supplies are available, until the vaccine has expired.
- Also available for those not eligible for free HPV vaccine through patient-pay (approximately $300 for the 3 doses).
- Indications for females aged between 9 and 45 for the prevention of:
|
Age at Time of Receipt of 1st Dose |
Recommended Vaccine (Number of Doses) |
Costs |
| 9 - 14* | Gardasil® (2 doses) | Publicly funded program |
|
15 - 19 |
Gardasil® (3 doses) |
|
|
20 - 26 |
Cervarix® (3 doses) or Gardasil® (3 doses) |
Cervarix® – Publicly funded by a one-time program |
|
> 26 |
Gardasil® (3 doses) or Cervarix® (3 doses) |
Patient pay |
|
> 45 |
Neither |
|
For more information on immunization and the vaccines, refer to 1) Appendix A: HPV Vaccine Descriptions (PDF, 112KB); 2) Public Health Agency of Canada, link: www.phac-aspc.gc.ca/; 3) BC Centre for Disease Control (BCCDC), link: www.bccdc.ca; or 4) ImmunizeBC, link: immunizebc.ca/.
Screening
Cervical Cancer
In BC, conventional Pap test (also known as cervical cytology) is currently the only test used for the cervical cancer screening program for asymptomatic females. Refer to Appendix B: Pap Sampling Technique (PDF, 294KB).
Other tests include liquid-based cytology (LBC) (which is currently unavailable in BC) and high-risk human papillomavirus (hrHPV) molecular testing (which is available in BC by patient pay).
Symptomatic women should be treated appropriately. If cancer of the cervix is clinically suspected, then refer to the nearest colposcopy clinic, even if there are negative screening results.
Age to Start Screening for Average Risk (as of June 2016)2
It is currently recommended that screening for cervical cancer should begin at age 25, including those who have received the HPV vaccine, in same sex relationship, or transgender with a cervix. Screening is not recommended for those aged 25 – 69 who
have never had sexual contact (i.e., intercourse, digital sexual contact, oral sexual contact) or patients after total hysterectomy (i.e., removal of cervix) but with no history of pre-cancerous lesions or cervical cancer.
Controversies in Care12
There are different recommendations on when to initiate screening for cervical cancer. These include starting at age 21, 25, or 30, or when a female becomes sexually active regardless of age. The Canadian Task Force on Preventive Health Care (CTFPHC)13 recommends routine screening should start at the age of 25 for those who are or have been sexually active. The age 25 is suggested because 1) invasive cervical cancers in females < 25 are rare; 2) screening methods are less effective in younger females; 3) the majority of oncogenic HPV infections as well as precursor lesions tend to resolve spontaneously in younger females; and 4) harms associated with screening and treating younger females (e.g., treatment of precursor lesions may be associated with an increased risk of preterm births).
Screening Intervals for Average Risk (as of June 2016)2
Repeat Pap tests every 3 years. An optimal screening interval will minimize the detection of transient cervical intraepithelial neoplasia (CIN) lesions, without exposing females to an unacceptably high risk of invasive cervical carcinoma.
Screening Intervals for Higher Risk (as of June 2016)2
- Immunocompromised individuals (includes those with human immunodeficiency virus [HIV/AIDS], lymphoproliferative disorders, organ transplants, and those under long-term immunosuppression therapy: Annual screening.
- History of pre-cancerous lesions or cervical cancer:
| History | Screening Recommendations |
| CIN 2+: treated (cone, LEEP, ablative therapy), HPV negative, discharge from colposcopy | Follow average risk guidelines. |
| CIN 2+: treated (cone, LEEP, ablative therapy), HPV positive, discharge from colposcopy | Annual screening until there are 3 no significantly abnormal* Pap tests within 5 years, and then follow average risk guidelines. |
| CIN 2+: untreated, regressed or discharged | Annual screening until there are 3 no significantly abnormal* Pap tests within 5 years, and then follow average risk guidelines. |
| CIN 2+: untreated and lost to follow-up | Refer to colposcopy for assessment. |
| Invasive Cervical Cancer and discharged from colposcopy or the BCCA | Annual screening until there are 3 no significantly abnormal* Pap tests within 5 years, and then follow average risk guidelines. |
| High-grade squamous intraepithelial lesion (HSIL): CIN 1 or negative at initial colposcopy, no subsequent biopsy or follow-up | Refer to colposcopy for assessment. |
| HSIL: CIN 1 or negative at colposcopy, discharge from colposcopy | Annual screening until there are 3 no significantly abnormal* Pap tests within 5 years, and then follow average risk guidelines. |
| Adenocarcinoma in situ (AIS) cytologic diagnosis. CIN 1 or negative at colposcopy, discharged from colposcopy | Annual screening until there are 3 no significantly abnormal* Pap tests within 5 years, and then follow average risk guidelines. |
- Hysterectomy with the cervix removed and a history of pre-cancerous lesions or cervical cancer:
| History | Screening Recommendations |
| Invasive cervical cancer Histologically proven CIN 2+ | Vaginal vault smear annually – for 25 years after the most recent histological evidence of CIN 2+ or vaginal intraepithelial neoplasia (VAIN) 2+. |
| HISL: CIN 1 or negative at colposcopy | Vaginal vault smear annually – for 25 years after the most recent HSIL. |
- High risk behaviours: Follow average risk guidelines.
Age to Stop Screening for Average Risk2
There is a lack of evidence for or against screening in older age groups. In BC, the current recommendation is that females should discontinue cervical cancer screening at age 69, provided that they have had at least three negative screening test results in the past 10 years and have not been previously treated for CIN or invasive cancer.
Age to Stop Screening for Higher Risk2
| Category | Screening Recommendations |
| Immunocompromised individuals | The benefits of screening beyond age 69 must be weighed in the context of the overall health of the patient. |
| History of pre-cancerous lesions or cervical cancer | Age 69 or 25 years since diagnosis with at least 5 negative Pap test with no significantly abnormality* in last 10 years whichever occurs later. |
| Hysterectomy with the cervix removed and a historyof pre-cancerous lesions or cervical cancer | |
| High risk behaviours | N/A |
*Significant abnormality is anything more severe than atypical squamous cells of undetermined significance (ASCUS) or low-grade squamous intraepithelial lesion (LSIL).
Vaginal and Vulvar Cancer
These areas should be examined during a gynecological examination for lesions or skin changes.
Diagnosis
Cervical Cancer
Recommendations for further investigations (e.g., colposcopy) or repeat testing will be provided on the cytology report for any abnormal Pap tests.
In the event of a clinical lesion, or if cancer of the cervix is clinically suspected, a Pap test is not an appropriate diagnostic procedure. Even in the case of a reassuring Pap test, if cancer of the cervix is clinically suspected, then arrange either a biopsy or colposcopy.
If invasive cervical cancer is diagnosed, then refer the patient to BCCA for assessment and management planning by a multidisciplinary team.* The benchmark for an appointment at BCCA is 2 weeks following referral; urgent cases may be seen sooner upon telephone consultation.
Vaginal and Vulvar Cancer
Diagnosis is made by vulvo-vaginal visualization, palpation and biopsy. Biopsy any suspicious lesions or refer to BCCA. Note that speculum blades may obscure full visualization of vaginal tissue.
Once diagnosed, refer the patient to BCCA for assessment and management planning by a multidisciplinary team.* The benchmark for an appointment at the BCCA is 2 weeks following referral; urgent cases may be seen sooner upon telephone consultation.
* This multidisciplinary team includes gynecologic oncologists (surgeons), radiation oncologists, medical oncologists, pathologists, radiologists, general practitioners in oncology, nurses, radiation therapists, counsellors and nutritionists.
Treatment
Treatment for cervical, vaginal and vulvar cancers will be directed by the BCCA team.
Cervical Cancer
Management will be surgical if the lesion is small with no extra-cervical disease, and with a low risk of lymph node metastasis. Radiation with concurrent chemotherapy is standard management for larger lesions.
Fertility-sparing surgery may be an option in some circumstances.
Vaginal Cancer
Lower vaginal cancers (i.e., lower 1/3) will mostly be treated with surgery. Radiation and concurrent chemotherapy may be advised in selected cases.
Upper vaginal cancers (i.e., upper 2/3) will mostly be treated with radiation and concurrent chemotherapy. Surgery may be appropriate in selected cases.
Vulvar Cancer
The specific surgical procedure may vary from a wide local excision to a radical approach. Surgery will be individualized, to preserve vital but uninvolved structures (such as sphincters and the clitoris), and to avoid radical groin resection. Sentinel node assessment is now the standard approach for lesions smaller than 2 cm.
Neoadjuvant radiotherapy (which is therapy given before surgery) may be used to downstage cancers that involve vital structures. When cancer involves vital structures such as the anus, uretha or clitoris, pre-surgical radiation may reduce the tumour size with the hope that these structures may be preserved at the time of surgery.
Adjuvant radiotherapy (which is therapy given after surgery) may be recommended after resection of involved inguinal nodes, or when surgical margins are close.
Follow-up
Once the patient has completed treatment, she will be discharged from the BCCA. Upon discharge, the family physician may be asked to manage the patient’s follow-up care.
Follow-up care includes:
- surveillance for recurrence or new cancer;
- monitoring and treating complications and/or side effects from treatment; and
- providing patient support.
Specific recommendations will be provided in the patient’s discharge letter. At any time, the patient and/or family physician may consult with the BCCA regarding any follow-up questions or concerns. If recurrent disease is suspected, then re-refer patient back to the BCCA.
Below are general recommendations for a patient’s follow-up visits with her family physician, based on the type of cancer and/or type of therapy.
Cervical Cancer14
The timing of the follow-up visits are:
- Year 1 = Every month for the first 3 months, then every 2 months
- Year 2 = Every 4 months
- Years 3, 4 & 5 = Every 6 months
- Years 5+ = Annually
A follow-up visit consists of:
- review of any symptoms (e.g., pain, discharge, vaginal bleeding, menopause, swelling of leg or vulva, new neurological lower limb symptoms, issues with sexual, urinary and/or bowel functions);
- physical exam, including lymph node surveillance (supraclavicular, inguinal and femoral nodes), abdomen, speculum and pelvic exam;
- cervical or vaginal vault screening as per screening guidelines; and
- any patient support required (e.g., counselling about sexual health - maintenance of vaginal patency post radiotherapy, through regular vaginal intercourse or the use of a dilator).
Vaginal Cancer15
The timing of the follow-up visits are:
- Year 1 = Every 3 months
- Year 2 = Every 4 months
- Years 3, 4 & 5 = Every 6 months
- Years 5+ = Annually
Vulvar Cancer16
1. Post surgical
The timing of the follow-up visits are:
- Year 1 = Every 4 months
- Years 2, 3, 4 & 5 = Every 6 months
- Years 5+ = Annually
2. Post radiotherapy
The timing of the follow-up visits are:
- Year 1 = First visit at 1 month, then every 2 months
- Years 2 & 3 = Every 6 months
- Years 3+ = Annually
A follow-up visit consists of a review of any symptoms; and a physical exam, including pelvic exam and Pap test.
Resources
References
- BC Cancer Agency. Cancer Management Guidelines - Gynecology – Uterine Cervix – 4.1 Predisposing Factors/Prevention [updated 2008; cited 2014 March].
- BC Cancer Agency. Screening for cancer of the cervix: An office manual for health professionals. 2016.
- Collins S, Rollason TP, Young LS, et al. Cigarette smoking is an independent risk factor for cervical intraepithelial neoplasia in young women: A longitudinal study. Eur J Cancer. 2010;46(2):405-411.
- International Collaboration of Epidemiological Studies of Cervical Cancer. Carcinoma of the cervix and tobacco smoking: Collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int J Cancer. 2006;118:1481-1495.
- Lam JU, Rebolj M, Dugue PA, et al. Condom use in prevention of human papillomavirus infections and cervical neoplasia: Systematic review of longitudinal studies. J Med Screen. 2014;21(1):38-50.
- Winer RL, Hughes JP, Feng Q, et al. Condom use and the risk of genital human papillomavirus infection in young women. N Engl J Med. 2006;354(25):2645-54.
- Public Health Agency of Canada. An Advisory Committee Statement (ACS) - National Advisory Committee on Immunization (NACI) - Update on Human Papillomavirus (HPV) Vaccine Immunization Schedule. CCDR. 2015.
- Merck Canada Inc. Product monograph: Gardasil® [Quadrivalent Human Papillomavirus (Types 6, 11, 16, 18) Recombinant Vaccine]. 2013 03/14.
- Immunize BC [Internet], British Columbia: BC Centre for Disease Control. Human Papillomavirus (HPV) Vaccine Extended Schedule: Health Care Professional Questions and Answers [updated July 2013; cited 2014 March].
- GlaxoSmithKline Inc. Product monograph: CERVARIX® Human Papillomavirus vaccine Types 16 and 18 (Recombinant, AS04 adjuvanted). 2013 05/02.
- Immunize BC [Internet], British Columbia: BC Centre for Disease Control. Ceravix® Clinical Questions and Answer Document [updated July 2013; cited 2014 March].
- Kruger H, Kwon J, Sadownik, L et al. What is the most appropriate age to start screening women for cervical cancer? BCMJ. 2013;55(6):282-286.
- Canadian Task Force on Preventive Health Care. Recommendations on screening for cervical cancer. CMAJ. 2013;185(1):35-45.
- BC Cancer Agency. Cancer Management Guidelines - Gynecology – Uterine Cervix – 4.6 Follow-up [cited 2014 April].
- BC Cancer Agency. Cancer Management Guidelines - Gynecology – Vagina – Follow-up [cited 2014 April].
- BC Cancer Agency. Cancer Management Guidelines - Gynecology – Vulva – 5.4 Follow-up [cited 2014 April].
Resources
- BC Cancer Agency, www.bccancer.bc.ca, which includes many patient resources.
- Division of Gynecologic Oncology, telephone 1-800-663-3333 (extensions 2353, 2365, or 2367)
- Cervix Cancer Screening in BC, www.screeningbc.ca/Cervix/default.htm
- Immunize BC, www.immunizeBC.ca
- For patients: https://immunizebc.ca/vaccines-by-disease
- BC Centre for Disease Control, www.bccdc.ca
- Public Agency of Canada, www.phac-aspc.gc.ca
- HealthlinkBC, www.healthlinkbc.ca or by telephone (toll free in BC) 8-1-1 or 7-1-1 (for the hearing impaired) for health information, translation services and dieticians
Appendices
- Appendix A: HPV Vaccine Descriptions (PDF, 112KB)
- Appendix B: Pap Sampling Technique (PDF, 294KB)
- Appendix C: Cervical Cytology Terminology used by BC Cervical Cancer Screening Program (PDF, 105KB)
Associated Documents
The following documents accompany this guideline:
- BCGuidelines.ca - Genital Tract Cancers in Females: Endometrial Cancer
- BCGuidelines.ca - Genital Tract Cancers in Females: Ovarian, Fallopian Tube, and Primary Peritoneal Cancers
This guideline is based on scientific evidence current as of the Effective Date.
This guideline was developed by the Family Practice Oncology Network and the Guidelines and Protocols Advisory Committee, approved by the British Columbia Medical Association, and adopted by the Medical Services Commission.
|
The principles of the Guidelines and Protocols Advisory Committee are to:
|
Disclaimer The Clinical Practice Guidelines (the "Guidelines") have been developed by the Guidelines and Protocols Advisory Committee on behalf of the Medical Services Commission. The Guidelines are intended to give an understanding of a clinical problem and outline one or more preferred approaches to the investigation and management of the problem. The Guidelines are not intended as a substitute for the advice or professional judgment of a health care professional, nor are they intended to be the only approach to the management of clinical problems. We cannot respond to patients or patient advocates requesting advice on issues related to medical conditions. If you need medical advice, please contact a health care professional.


 TOP
TOP